✅ Just Accepted
⭐ Editor's Choice
#IDSky
✅ Just Accepted
⭐ Editor's Choice
#IDSky
✅ Just Accepted
#IDSky

✅ Just Accepted
#IDSky
www.thelancet.com/journals/lan...

www.thelancet.com/journals/lan...
Meropenem & pip/tazo optimised dosing regimens for critically ill patients receiving RRT
Dosing nomograms developed to inform dosing for different RRT settings, urine outputs & target conc #idsky
link.springer.com/article/10.1...



Meropenem & pip/tazo optimised dosing regimens for critically ill patients receiving RRT
Dosing nomograms developed to inform dosing for different RRT settings, urine outputs & target conc #idsky
link.springer.com/article/10.1...
We study the interaction between misinformation and science on Twitter during COVID-19 based on ~407M tweets. Both science and misinformation featured prominently during the pandemic, but the interaction between the two has not been studied on this scale before.
🧵 (1/10)
We study the interaction between misinformation and science on Twitter during COVID-19 based on ~407M tweets. Both science and misinformation featured prominently during the pandemic, but the interaction between the two has not been studied on this scale before.
🧵 (1/10)

#MedSky + #IDSky + #PedSky via @cnn.com -
www.cnn.com/2025/07/05/h...

#MedSky + #IDSky + #PedSky via @cnn.com -
www.cnn.com/2025/07/05/h...
(TBH, this is appilicable to all blood stream infections!)
#IDSky #ClinMicro #AMR
(TBH, this is appilicable to all blood stream infections!)
#IDSky #ClinMicro #AMR
www.cidrap.umn.edu/adult-non-fl...

www.cidrap.umn.edu/adult-non-fl...
This SR of observational studies shows:
✅ Clinical cure >70%
⚠️ Relapses up to 50% at 6 month
💩 Frequent diarrhea
link.springer.com/article/10.1... #AMSsky #UTIsky #IDsky

This SR of observational studies shows:
✅ Clinical cure >70%
⚠️ Relapses up to 50% at 6 month
💩 Frequent diarrhea
link.springer.com/article/10.1... #AMSsky #UTIsky #IDsky
www.cidrap.umn.edu/healthcare-a...
Members have expertise in IDs, infection prevention and control, healthcare epidemiology, nursing, public health, and other areas of health and medicine #IDsky #Medsky

www.cidrap.umn.edu/healthcare-a...
Members have expertise in IDs, infection prevention and control, healthcare epidemiology, nursing, public health, and other areas of health and medicine #IDsky #Medsky
#MedSky #pedsky #cardiosky #cansky #obgynsky #immunosky #episky #nephsky

#MedSky #pedsky #cardiosky #cansky #obgynsky #immunosky #episky #nephsky
www.thelancet.com/journals/lan...
#hepsky #liversky #medsky #idsky
www.thelancet.com/journals/lan...
#hepsky #liversky #medsky #idsky
www.healio.com/news/infecti...
#hepsky #idsky #liversky #medsky via @gohealio.bsky.social
www.healio.com/news/infecti...
#hepsky #idsky #liversky #medsky via @gohealio.bsky.social
▶️ Critically ill opioid use disorder (OUD) patients face high MDRO infection rates (22.5%), with MRSA most common
▶️ Key risk factors include housing insecurity, lack of OUD meds, HCV status, and recent IV antibiotic use.
#IDSky
📄: doi.org/10.1017/ice....
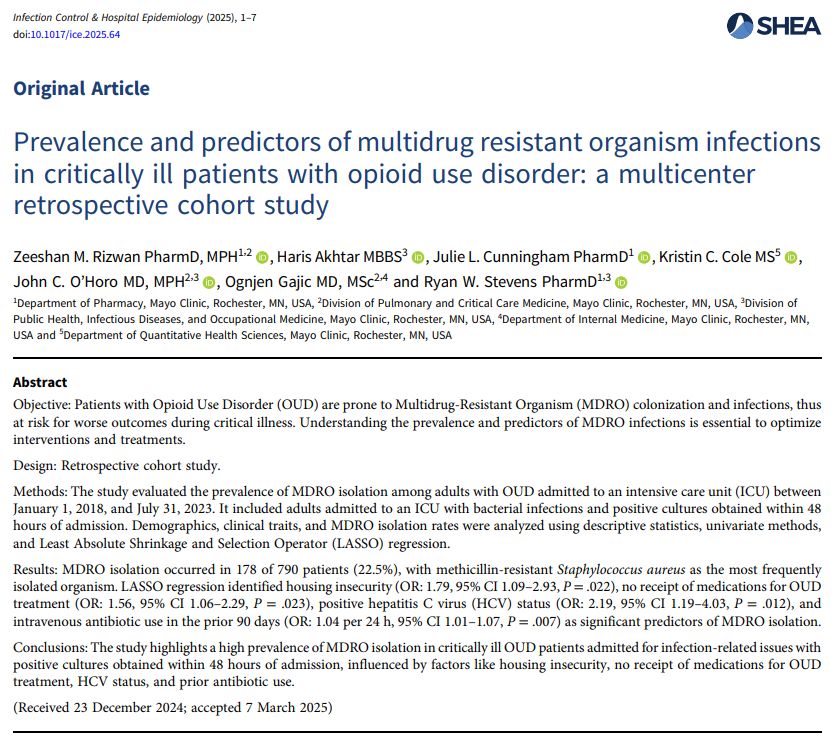
▶️ Critically ill opioid use disorder (OUD) patients face high MDRO infection rates (22.5%), with MRSA most common
▶️ Key risk factors include housing insecurity, lack of OUD meds, HCV status, and recent IV antibiotic use.
#IDSky
📄: doi.org/10.1017/ice....
www.sciencedirect.com/science/arti...

www.sciencedirect.com/science/arti...
This study shows a time- and dose-dependent association between PPI & steroids and the incidence of HAIs: www.journalofhospitalinfection.com/callback?red...
#AMSky #IDsky #IPSky #PharmSky

This study shows a time- and dose-dependent association between PPI & steroids and the incidence of HAIs: www.journalofhospitalinfection.com/callback?red...
#AMSky #IDsky #IPSky #PharmSky


