7% said it led or contributed to a patient’s death.
This data is clear.
We need to #fixPriorAuth
www.astro.org/news-and-pub...

7% said it led or contributed to a patient’s death.
This data is clear.
We need to #fixPriorAuth
www.astro.org/news-and-pub...
"Fax from the pharmacy for Duloxetine 40mg caps stating this is not covered. Per insurance, this drug requires a PA. Please consider switching to Duloxetine 20mg caps taking 2 a day."
"Fax from the pharmacy for Duloxetine 40mg caps stating this is not covered. Per insurance, this drug requires a PA. Please consider switching to Duloxetine 20mg caps taking 2 a day."
PET scan appointment available Monday but was told it would be at least 2 weeks because of #priorauth
This is not how it is supposed to work
@MedicineForward
PET scan appointment available Monday but was told it would be at least 2 weeks because of #priorauth
This is not how it is supposed to work
@MedicineForward
INSULIN GLARGINE.
What in the actual bleeping bleep bleep.
Incidentally, patient has UHC.
Unacceptable.
#medsky #endocrinesky #primarycare
INSULIN GLARGINE.
What in the actual bleeping bleep bleep.
Incidentally, patient has UHC.
Unacceptable.
#medsky #endocrinesky #primarycare
We have nothing else to do with our time, do we? #CVprev #priorauth #cardiosky

Read more (published October) ⬇️

Read more (published October) ⬇️


I did everything I was asked
This is a necessary generic med
The system is broken
I am broken
Just filled out this form to fax back with the route of administration and the diagnosis code
Reader, both of those data points ARE ON THE ORIGINAL PRESCRIPTION
We are 6 days beyond me calling them
The levels of needless hoop jumping is maddening
I did everything I was asked
This is a necessary generic med
The system is broken
I am broken


Patient with invasive fungal infection who needs Cresemba. Denied. You can use fluconazole (which doesn't work for anything other than candida).
Patient with invasive fungal infection who needs Cresemba. Denied. You can use fluconazole (which doesn't work for anything other than candida).



41 prior auths per doctor per week
13 hours spent per week on prior auths
24% reported hospitalizations due to delays from prior auths
8% reported disability/deaths due to delays from prior auths
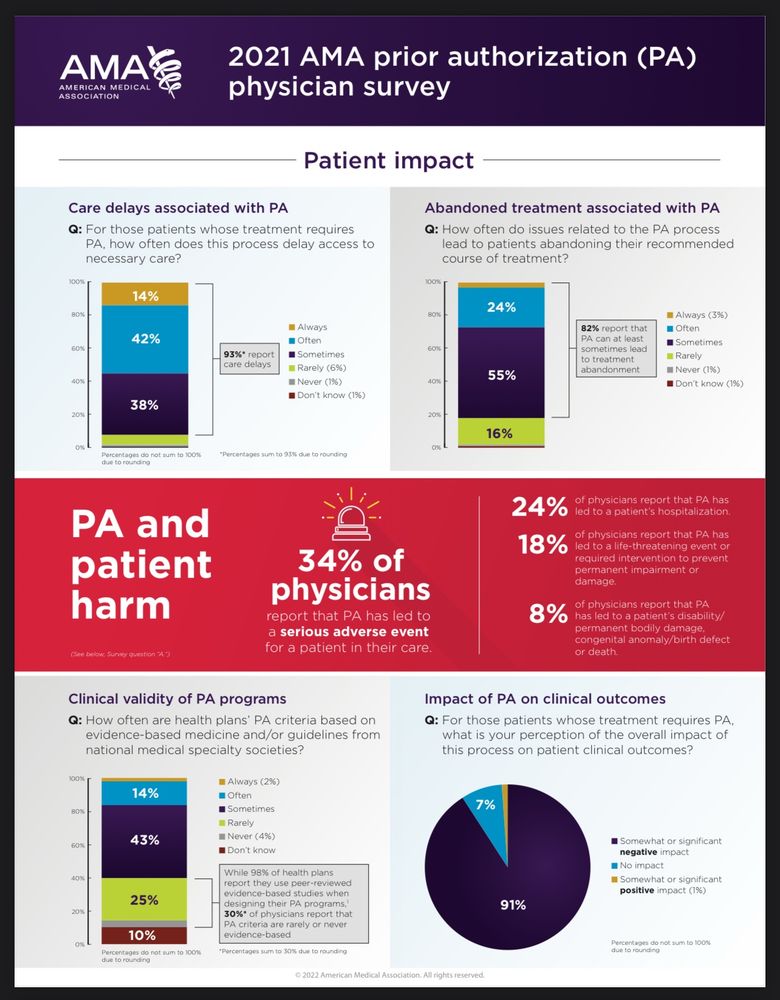
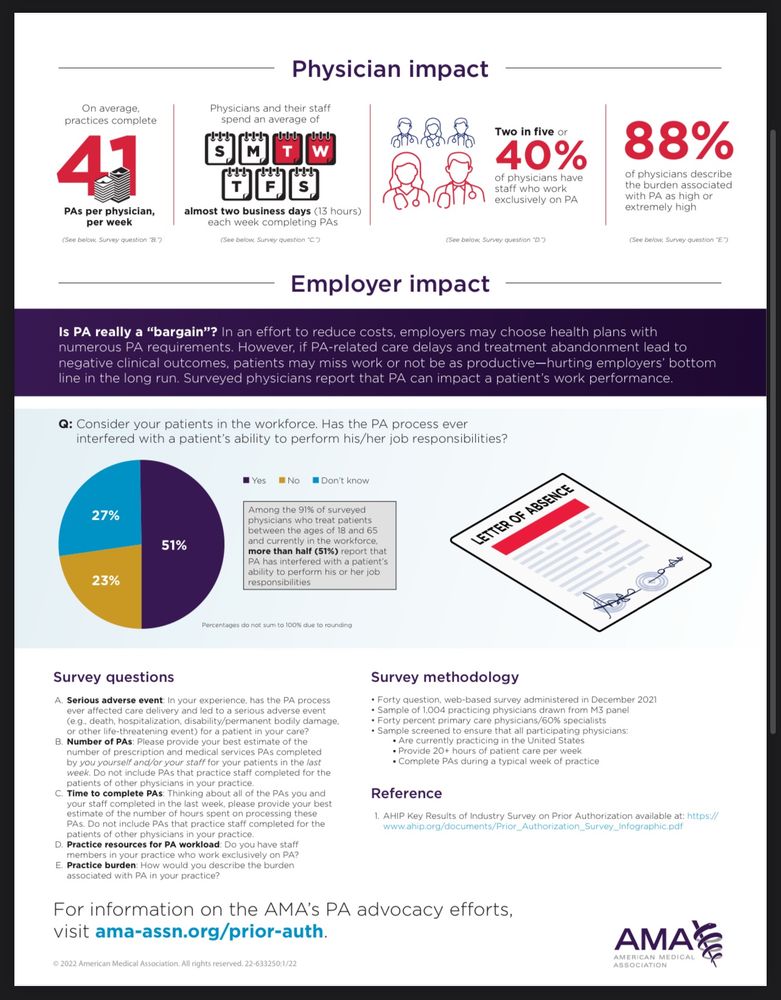
41 prior auths per doctor per week
13 hours spent per week on prior auths
24% reported hospitalizations due to delays from prior auths
8% reported disability/deaths due to delays from prior auths



