
Passionate about gastrointestinal dysfunction, nutrition as well as ECMO and cardiopulmonary physiology. Enthusiast in #MatLab, signal analysis and data-driven research: https://pubmed.ncbi.nlm.nih.gov/?term=Kaspar+bachman
fluclox caused more acute kidney injury than cefazolin; early mortality favored cefazolin
Absolutely Herculean effort by the entire global trial team and practice changing data #teamcefazolin
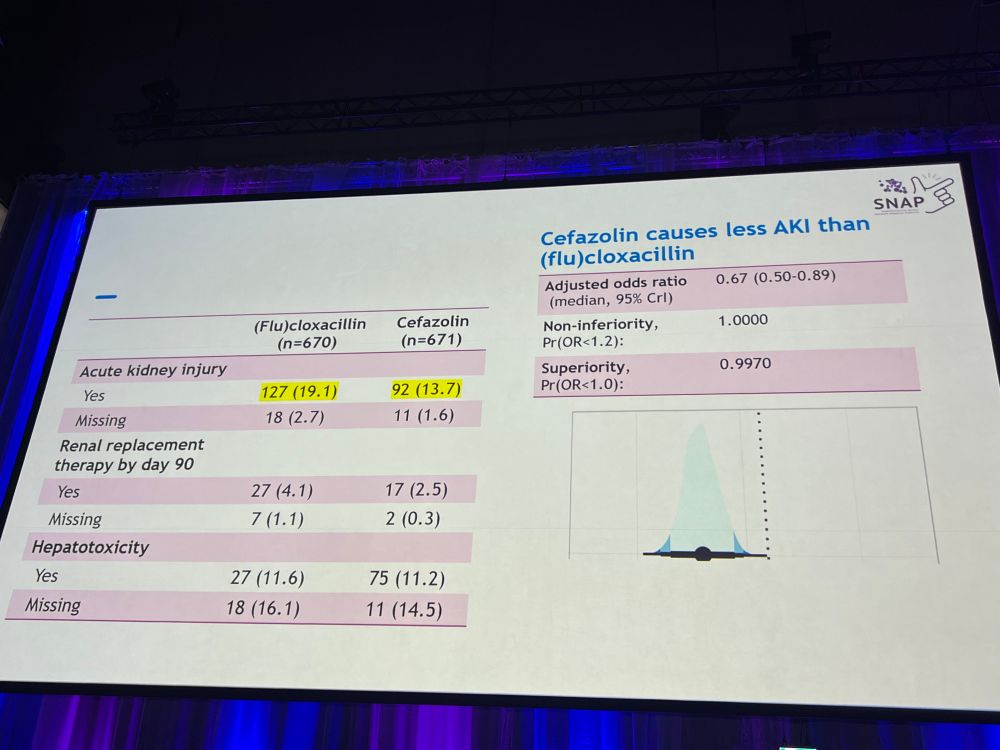
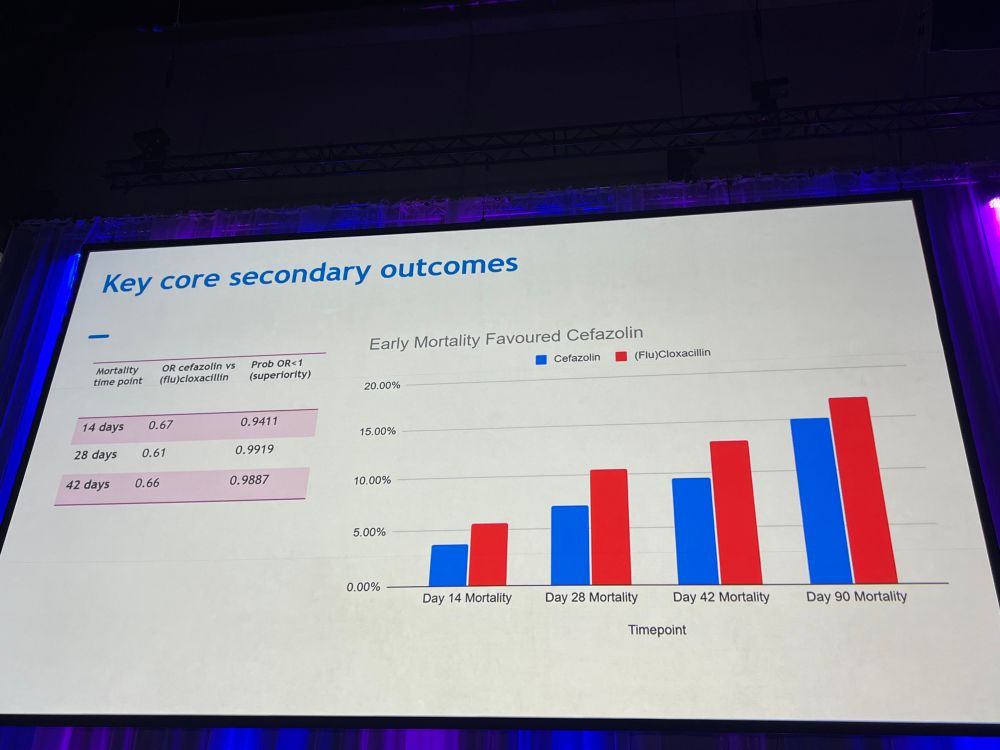
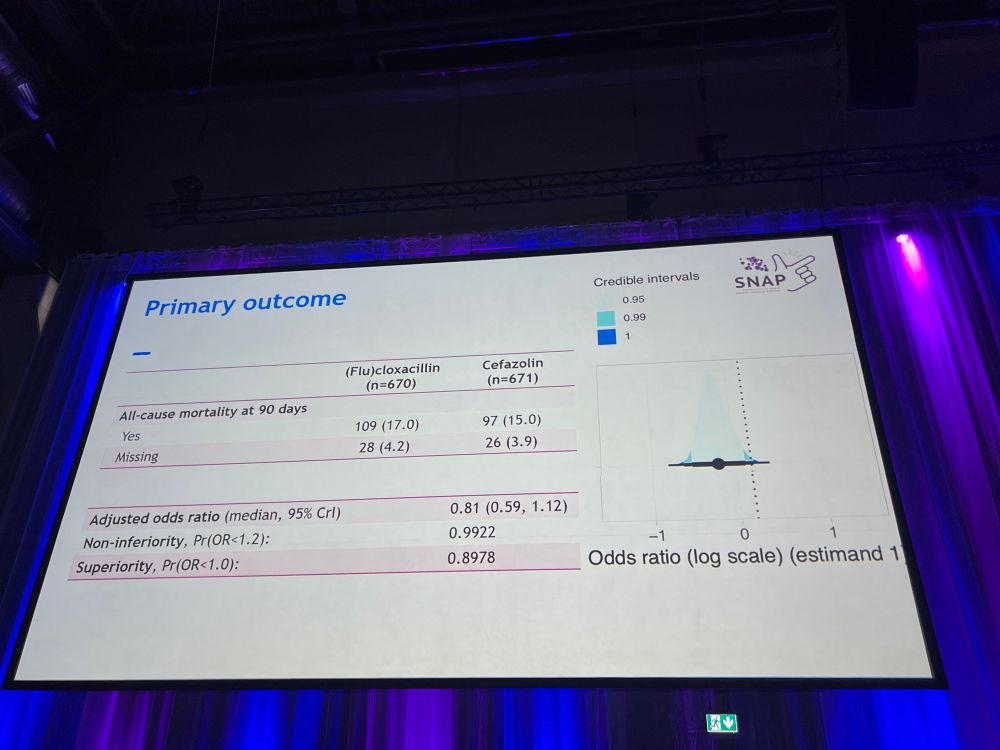
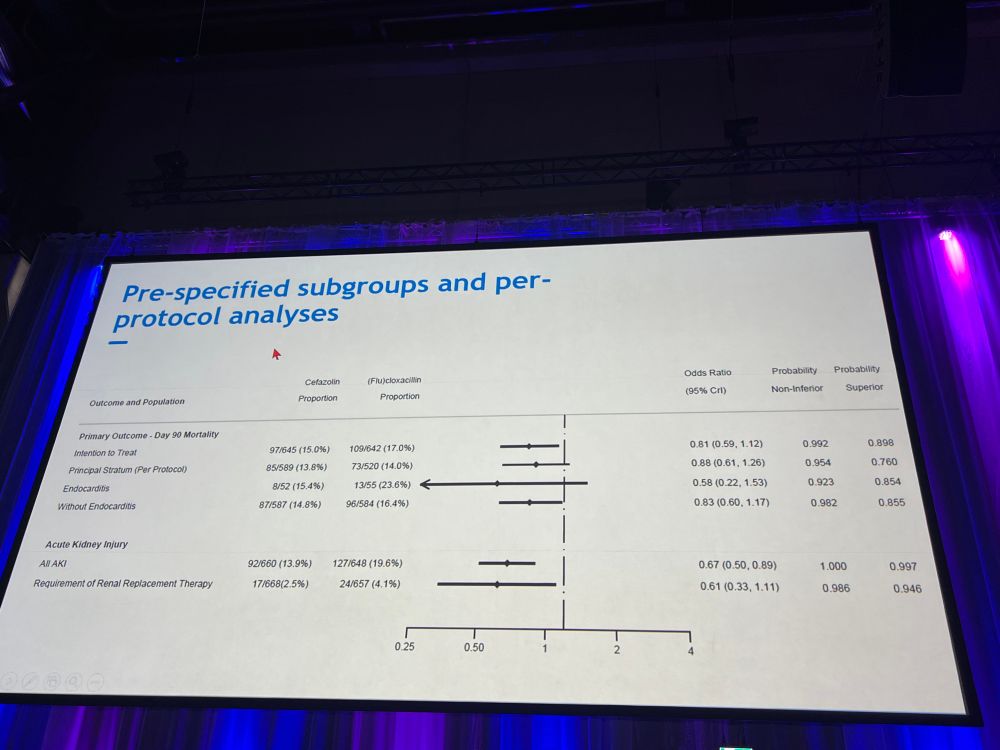
fluclox caused more acute kidney injury than cefazolin; early mortality favored cefazolin
Absolutely Herculean effort by the entire global trial team and practice changing data #teamcefazolin
soundphysicians.com/podcast-epis...
Has some good pearls and pitfalls and some resources in the shownotes.
soundphysicians.com/podcast-epis...
Has some good pearls and pitfalls and some resources in the shownotes.
We could then use that to 1) validate and 2) develop new models.
We could then use that to 1) validate and 2) develop new models.
I plan to do a thread on the paper/topic soon. This project has kept me busy over the last two years and it has been a pleasure working alongside an awesome steering committee and Delphi panel. 🙏
I plan to do a thread on the paper/topic soon. This project has kept me busy over the last two years and it has been a pleasure working alongside an awesome steering committee and Delphi panel. 🙏

