VortexApproach.org
UniversalAirway.org
SafeAirwaySociety.org
EZDrugID.org

Otherwise pancuronium.

Otherwise pancuronium.

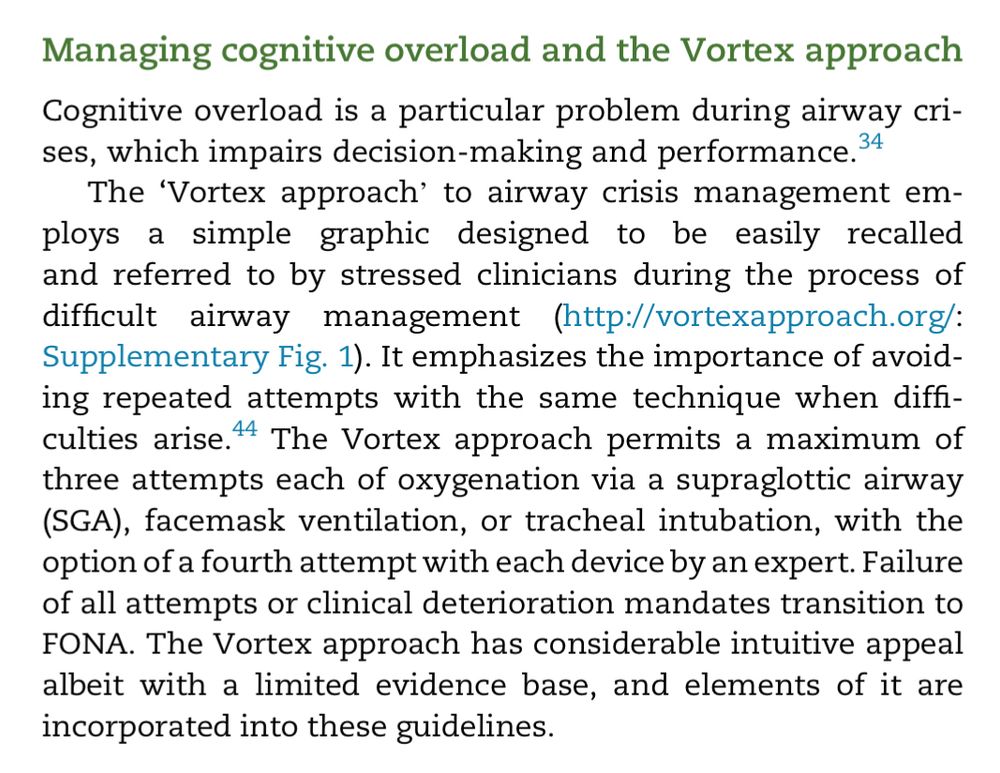
1. Acknowledging the utility of the Vortex graphic as an adjunct to facilitate implementation of the guidelines.
2. The ability to approach choice of rescue lifelines non-linearly.
3. Prompts to optimise attempts

1. Acknowledging the utility of the Vortex graphic as an adjunct to facilitate implementation of the guidelines.
2. The ability to approach choice of rescue lifelines non-linearly.
3. Prompts to optimise attempts



das.uk.com/guidelines/d...
das.uk.com/guidelines/g...




das.uk.com/guidelines/d...
das.uk.com/guidelines/g...
This study shows middle cerebral artery blood flow velocity decreases 50% w *MAP* < 60mmHg
pubmed.ncbi.nlm.nih.gov/26879693/

This study shows middle cerebral artery blood flow velocity decreases 50% w *MAP* < 60mmHg
pubmed.ncbi.nlm.nih.gov/26879693/
pubmed.ncbi.nlm.nih.gov/38205585/

pubmed.ncbi.nlm.nih.gov/38205585/
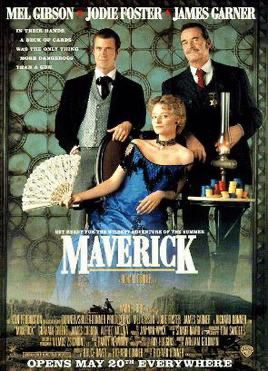
![Merely giving the patient
information, rather than expert guidance, may produce
suboptimal decisions and unnecessary stress [21].
Preserving patient autonomy is achieved by ensuring a
patient’s care aligns with their personal values. Whether any
outcome constitutes a material risk to a particular individual
is influenced by an array of factors, including personality;
experience; culture; age; sex; career; and lifestyle. It is
important that the anaesthetist has the ability to recognise
when patient values and priorities differ from their own.
Determining this essentially requires a reversal of the flow of
information; rather than providing information so that the
patient can make decisions, the emphasis should be on
acquiring information so that the clinician can make
management decisions in line with the patient’s stated
values. This information may be derived during the consent
process, elsewhere in the patient consultation or from other
sources.](https://cdn.bsky.app/img/feed_thumbnail/plain/did:plc:zbaj5jk7jtux3cccy6owpofu/bafkreibb3ny4wfkeil7jwzhwrwjz6v4nbet4fdnwuhfa6iimlvrssy7fjm@jpeg)


![rpretive model´ [23] aligns with anaesthetic
care as it describes a circumstance where the patient is often
unaware of the relevant information and how their values
might affect the delivery of care. It allows the clinician to
determine the vulnerabilities and concerns of an individual
and then use their expertise to deliver the most appropriate
care, augmenting rather than diminishing patient
autonomy. This is consistent with the concept of autonomy
as a multidimensional capacity, requiring not only the
cognitive ability to make rational decisions but additional
aspects such as understanding, intentionality and freedom
from external constraints, which the patient may require
support from others to attain](https://cdn.bsky.app/img/feed_thumbnail/plain/did:plc:zbaj5jk7jtux3cccy6owpofu/bafkreiftrspmz2pzputq3ff3cfgcsmxk6farr2fy2n3quhgx74lc5jdvsq@jpeg)
1. You don’t necessarily have to have the surgery.
2. Even if you do have the surgery there are multiple ways to do the same thing, each with different risks, that can be chosen according to complications which the patient is particularly vulnerable to or concerned about.

1. You don’t necessarily have to have the surgery.
2. Even if you do have the surgery there are multiple ways to do the same thing, each with different risks, that can be chosen according to complications which the patient is particularly vulnerable to or concerned about.
(actually I loved the Rockford Files speaking of James Garner)
(actually I loved the Rockford Files speaking of James Garner)

We speculate that it may be easier for pts to conceptualise likelihood if descriptors are framed in terms of how often clinicians encounter them cf proportion of pts experiencing them.

We speculate that it may be easier for pts to conceptualise likelihood if descriptors are framed in terms of how often clinicians encounter them cf proportion of pts experiencing them.
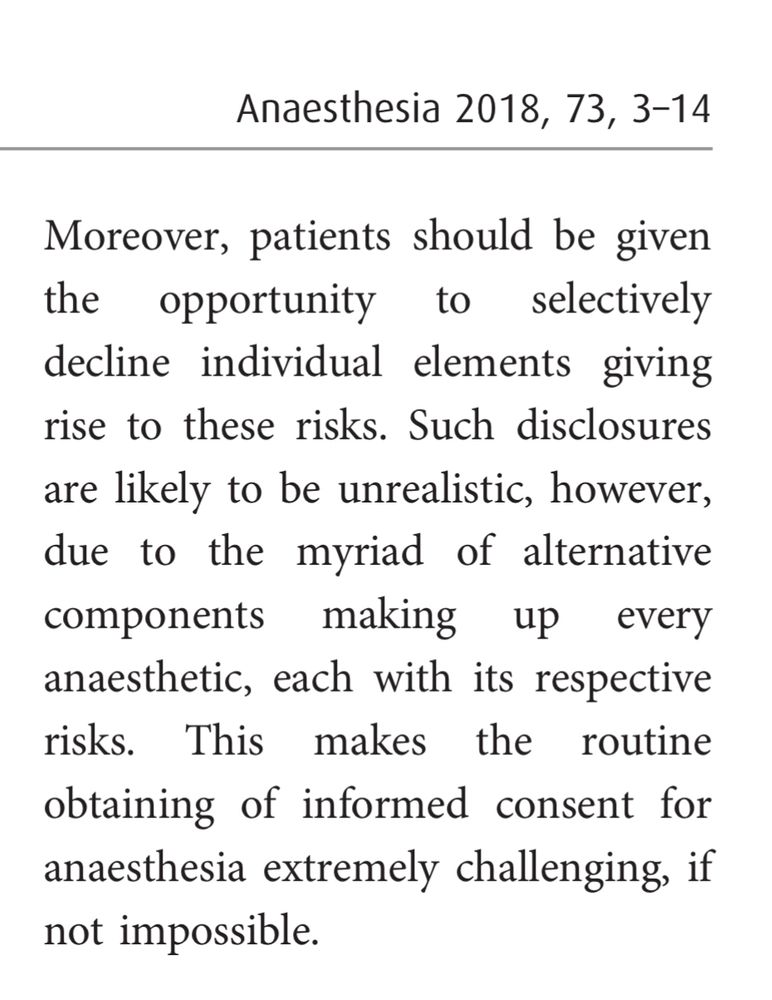
From ‘The paradox of informed consent’. Free for a limited time in @anaesjournal.bsky.social 🔓🔑⏳
associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/abs/10.1...

From ‘The paradox of informed consent’. Free for a limited time in @anaesjournal.bsky.social 🔓🔑⏳
associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/abs/10.1...
(while 70L/min mouth open is consistently crap)



(while 70L/min mouth open is consistently crap)
‘The paradox of informed consent’
Free full text in @anaesjournal.bsky.social for a limited time.
associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/abs/10.1...

‘The paradox of informed consent’
Free full text in @anaesjournal.bsky.social for a limited time.
associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/abs/10.1...
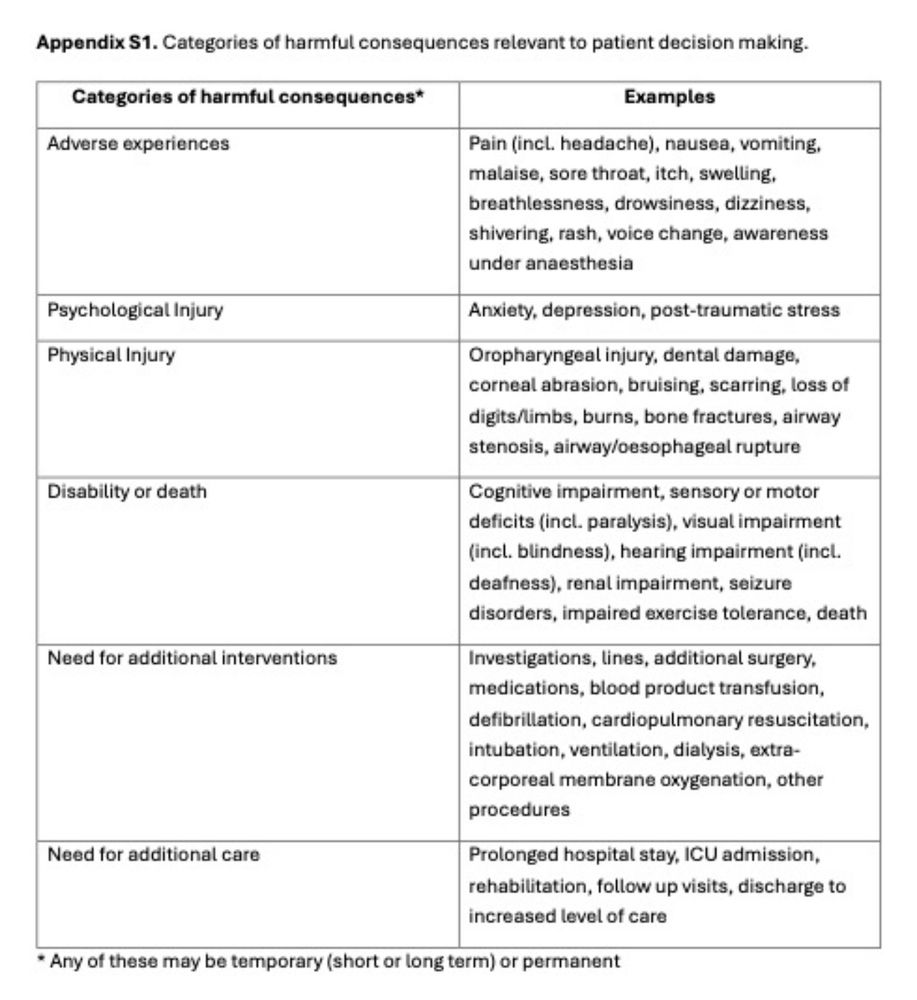
Perhaps we need to consent for consequences to the patient instead.

Perhaps we need to consent for consequences to the patient instead.
Even after 3 got altered & 4 added w the Samsoon modification in 1987, I’ve never heard of the tonsils getting involved!
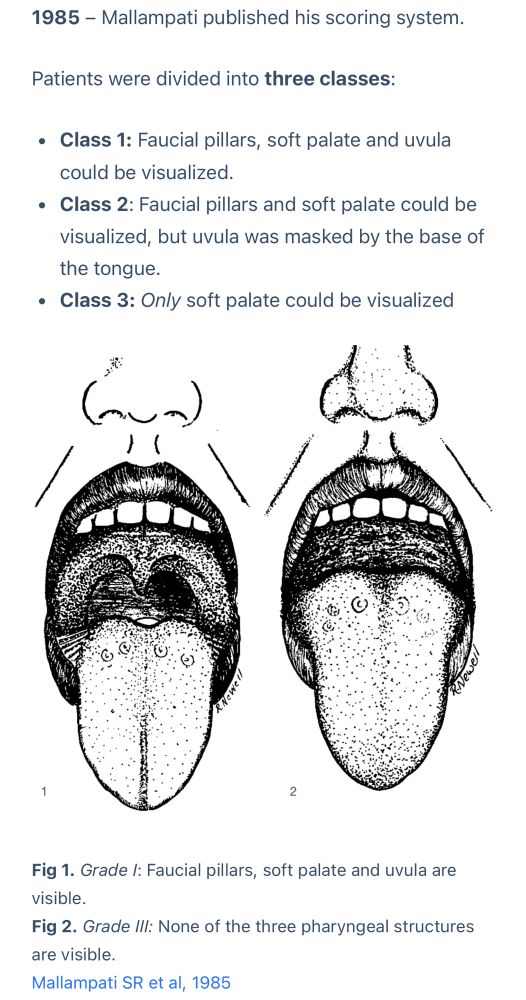

Even after 3 got altered & 4 added w the Samsoon modification in 1987, I’ve never heard of the tonsils getting involved!
I love “fair interrater reliability beyond that expected by chance”. Really setting a low bar there.
ASA Status, not perfect but better than a coin toss!




I love “fair interrater reliability beyond that expected by chance”. Really setting a low bar there.
ASA Status, not perfect but better than a coin toss!