We refuse to stand by while America’s public health safeguards are torn apart. bit.ly/4lm7UkW
We refuse to stand by while America’s public health safeguards are torn apart. bit.ly/4lm7UkW
transplantid.net "GUIDELINES"▶️ "ASTCT Guidelines"📁
#️⃣ 🔟 : Management of parainfluenza and hMPV after HSCT and CAR-T
Thanks Aneela Majeed @clevelandclinic.bsky.social!
transplantid.net/5WJIIMGH

transplantid.net "GUIDELINES"▶️ "ASTCT Guidelines"📁
#️⃣ 🔟 : Management of parainfluenza and hMPV after HSCT and CAR-T
Thanks Aneela Majeed @clevelandclinic.bsky.social!
transplantid.net/5WJIIMGH
Learn more about its broad clinical presentations, risk factors and management strategies, with this #EdsChoice review.
👉 buff.ly/GQHzurR
#IDSky #MedSky #CMV

Learn more about its broad clinical presentations, risk factors and management strategies, with this #EdsChoice review.
👉 buff.ly/GQHzurR
#IDSky #MedSky #CMV
✅ Just Accepted
#IDSky

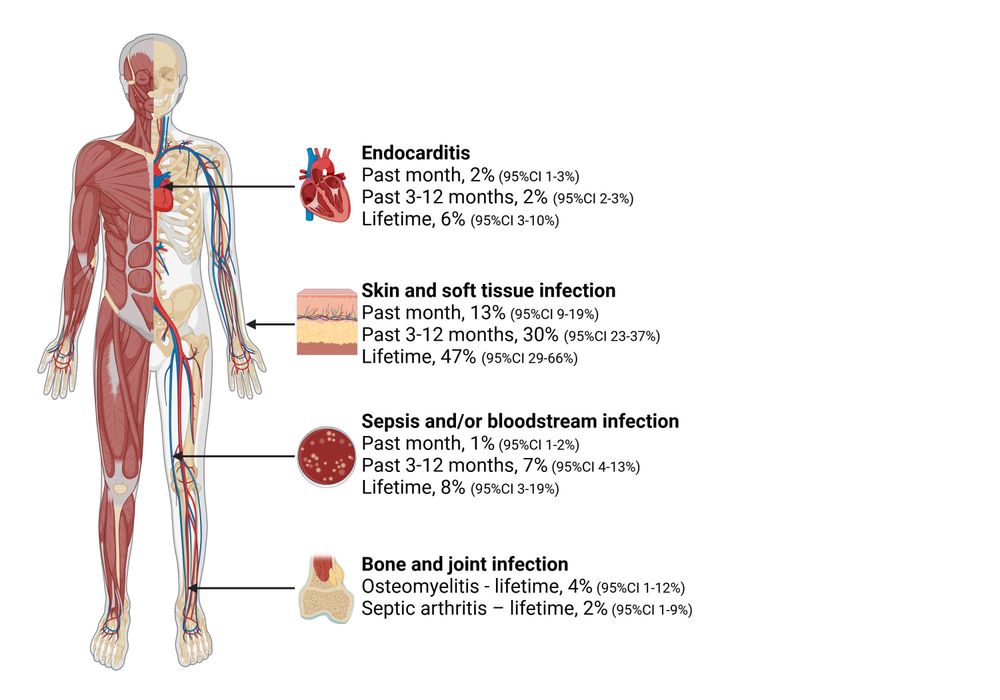
Infections:
academic.oup.com/jid/article/...

Infections:
academic.oup.com/jid/article/...
✅ Just Accepted
#IDSky


For years, TMP-SMX was the go-to, but alternatives are needed.
🧵(1/6)
For years, TMP-SMX was the go-to, but alternatives are needed.
🧵(1/6)
J Roberts etc
TLDR: ++variable, need tailored approach w TDM
link.springer.com/article/10.1...

J Roberts etc
TLDR: ++variable, need tailored approach w TDM
link.springer.com/article/10.1...
www.technologynetworks.com/tn/news/stra...
Something cool and scary to read this morning.

www.technologynetworks.com/tn/news/stra...
Something cool and scary to read this morning.
✅ Just Accepted
#IDSky

✅ Just Accepted
#IDSky
Outcomes of 56 kidney transplant recipients whose donors had positive BCx. Most pathogenic organisms were treated, while most commensals were not. No infections developed in recipients related to bacteremia
#IDSky #TxID
academic.oup.com/ofid/article...

Outcomes of 56 kidney transplant recipients whose donors had positive BCx. Most pathogenic organisms were treated, while most commensals were not. No infections developed in recipients related to bacteremia
#IDSky #TxID
academic.oup.com/ofid/article...
✅ Just Accepted
#IDSky

#AMR #IDSky #ClinMicro @cidjournal.bsky.social
academic.oup.com/cid/advance-...

#AMR #IDSky #ClinMicro @cidjournal.bsky.social
academic.oup.com/cid/advance-...
✅ Just Accepted
#IDSky
✅ Just Accepted
#IDSky

Can you give the MMR vaccine early in HSCT?
Short answer yes..study had a patient get it at day 300 post transplant. #IDsky #IDOnc

Can you give the MMR vaccine early in HSCT?
Short answer yes..study had a patient get it at day 300 post transplant. #IDsky #IDOnc
Global spatiotemporal dynamics of #Mycoplasma pneumoniae re-emergence after #COVID-19 pandemic restrictions: an epidemiological and transmission modelling study
www.thelancet.com/journals/lan...
#IDSky #ClinMicro #OpenAccess #OA

Global spatiotemporal dynamics of #Mycoplasma pneumoniae re-emergence after #COVID-19 pandemic restrictions: an epidemiological and transmission modelling study
www.thelancet.com/journals/lan...
#IDSky #ClinMicro #OpenAccess #OA
I spoke to a member of the FDA vaccine committee who confirmed that the meeting to decide the 2025-2026 flu shot composition was abruptly canceled today.
My on-the-record Q&A with the FDA advisor:
insidemedicine.substack.com/p/scoop-fda-...

I spoke to a member of the FDA vaccine committee who confirmed that the meeting to decide the 2025-2026 flu shot composition was abruptly canceled today.
My on-the-record Q&A with the FDA advisor:
insidemedicine.substack.com/p/scoop-fda-...

