
Member Executive Committee @kdigo.org Member #SLANH #AKI committee
Views do not represent those of my employer
#KidneyRunner 🏃🏻♂️ #StopAKI
Recently discussed my chapter on kidney disease from herbal medicine with our fellows—2 days later we saw an AKI case linked to these products.
We must ask about herbal meds/supplements routinely. #AKI #CKD








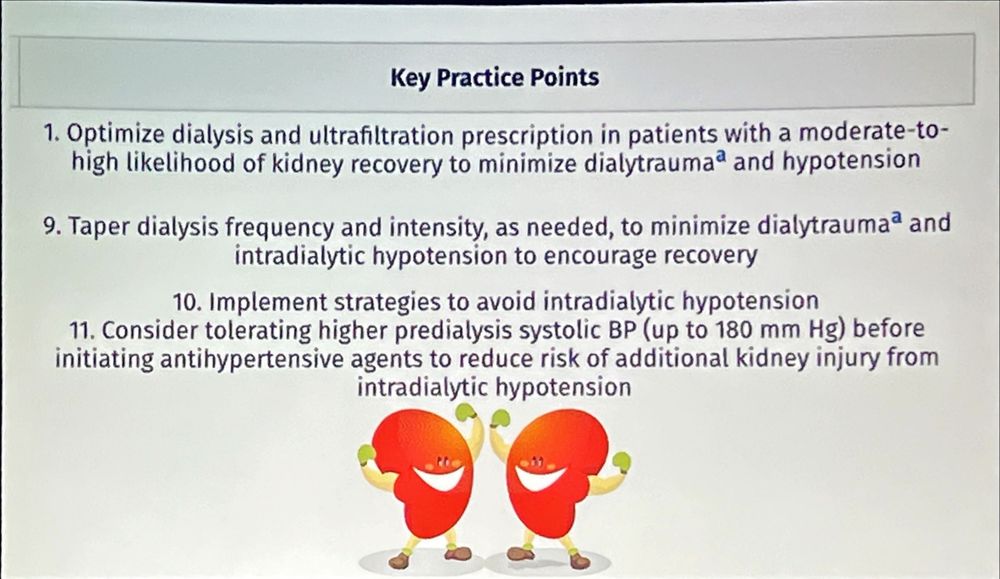
•Gentle UF & individualized Rx-minimize dialytrauma
•⬇️frequency/intensity as recovery starts
•Prevent IDH: 🆒 dialysate + slower UF
•Consider tolerating pre-HD SBP 🆙 to 180 mmHg before starting antihypertensives to avoid recurrent AKI & aid ❤️🩹#KidneyWk


•Gentle UF & individualized Rx-minimize dialytrauma
•⬇️frequency/intensity as recovery starts
•Prevent IDH: 🆒 dialysate + slower UF
•Consider tolerating pre-HD SBP 🆙 to 180 mmHg before starting antihypertensives to avoid recurrent AKI & aid ❤️🩹#KidneyWk


• Patient—older age, female, minority status, CKD/proteinuria, HF/CVD
• Meds—nephrotoxins
• Dialysis—↑UF/UFR, longer sessions, IDH
• SDOH—neighborhood poverty, dual-eligibility
(Babroudi et al., JASN 2024) #KidneyWk




• Patient—older age, female, minority status, CKD/proteinuria, HF/CVD
• Meds—nephrotoxins
• Dialysis—↑UF/UFR, longer sessions, IDH
• SDOH—neighborhood poverty, dual-eligibility
(Babroudi et al., JASN 2024) #KidneyWk

💧 Balanced crystalloids: modest survival benefit.
💉 IV bicarbonate: no survival advantage in severe acidosis overall.
⚠️ But in KDIGO stage 2–3 AKI + acidosis, may delay or reduce KRT need.
The story of bicarb continues… #AKI #CriticalCare

💧 Balanced crystalloids: modest survival benefit.
💉 IV bicarbonate: no survival advantage in severe acidosis overall.
⚠️ But in KDIGO stage 2–3 AKI + acidosis, may delay or reduce KRT need.
The story of bicarb continues… #AKI #CriticalCare
Event rates lower than expected, 15% crossover (controls got bicarb, 50% KRT).
KRT reduction remains provocative—true renal protection or just buying time?
Still not powered for MAKE-90.
More data coming from MOSAICC & SODa-BIC!
#KidneyWk

Event rates lower than expected, 15% crossover (controls got bicarb, 50% KRT).
KRT reduction remains provocative—true renal protection or just buying time?
Still not powered for MAKE-90.
More data coming from MOSAICC & SODa-BIC!
#KidneyWk


389 adults with severe acidemia randomized to 4.2% IV bicarb vs usual care. Overall primary outcome neutral, but in AKI stage 2–3 bicarb ↓ composite events, mortality, organ failure & KRT use (52%→35%). More alkalosis, hyperNa, hypoCa. #KidneyWk



389 adults with severe acidemia randomized to 4.2% IV bicarb vs usual care. Overall primary outcome neutral, but in AKI stage 2–3 bicarb ↓ composite events, mortality, organ failure & KRT use (52%→35%). More alkalosis, hyperNa, hypoCa. #KidneyWk







90-day mortality 21.8% vs 22.0% (OR 0.99); new RRT 12.7% vs 12.9%; max ↑SCr 0.41 vs 0.41 mg/dL.
Bottom line: no difference. #KidneyWk


90-day mortality 21.8% vs 22.0% (OR 0.99); new RRT 12.7% vs 12.9%; max ↑SCr 0.41 vs 0.41 mg/dL.
Bottom line: no difference. #KidneyWk
Plasma-Lyte 🆚 0.9% saline (fast vs slow).
90-day mortality 26.4% vs 27.2% (HR 0.97) → no overall difference; AKI/RRT/SOFA 🟰.
Post-hoc: if pre-enrollment💧were balanced, mortality likely ↓ (92% overall; 96% sepsis). TBI signal harm. #KidneyWk



Plasma-Lyte 🆚 0.9% saline (fast vs slow).
90-day mortality 26.4% vs 27.2% (HR 0.97) → no overall difference; AKI/RRT/SOFA 🟰.
Post-hoc: if pre-enrollment💧were balanced, mortality likely ↓ (92% overall; 96% sepsis). TBI signal harm. #KidneyWk



CVP: simple trends, poor for fluid responsiveness. PAC: full hemodynamics but invasive; static pressures not predictive. TPTD: CO/GEDV/EVLW—useful but invasive. PWCA: continuous dynamic indices; limits with arrhythmias/vaso-tone. #KidneyWk

CVP: simple trends, poor for fluid responsiveness. PAC: full hemodynamics but invasive; static pressures not predictive. TPTD: CO/GEDV/EVLW—useful but invasive. PWCA: continuous dynamic indices; limits with arrhythmias/vaso-tone. #KidneyWk
Exam/CXR/BNP → poor for venous congestion. Lung+IVC US better; VExUS best—predicts AKI/HF events & guides decongestion. BIA/BIVA trend TBW/edema but can’t split intravascular vs interstitial; ↓accuracy in obesity. #KidneyWk

Exam/CXR/BNP → poor for venous congestion. Lung+IVC US better; VExUS best—predicts AKI/HF events & guides decongestion. BIA/BIVA trend TBW/edema but can’t split intravascular vs interstitial; ↓accuracy in obesity. #KidneyWk










