🔹 Zhao, ARD 2023 🇨🇳: early use ↓proteinuria, ↓anti-dsDNA, improved podocyte autophagy. doi.org/10.1136/ard-...
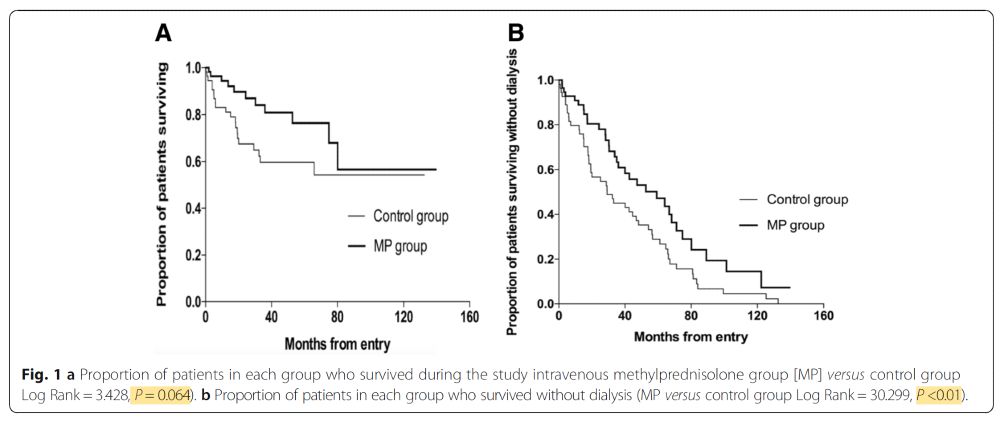
🔹 Vilardell-Vilà, KI 2025 🇪🇸: no benefit when started during active nephritis. doi.org/10.1016/j.ki...


🔹 Zhao, ARD 2023 🇨🇳: early use ↓proteinuria, ↓anti-dsDNA, improved podocyte autophagy. doi.org/10.1136/ard-...
🔹 Vilardell-Vilà, KI 2025 🇪🇸: no benefit when started during active nephritis. doi.org/10.1016/j.ki...










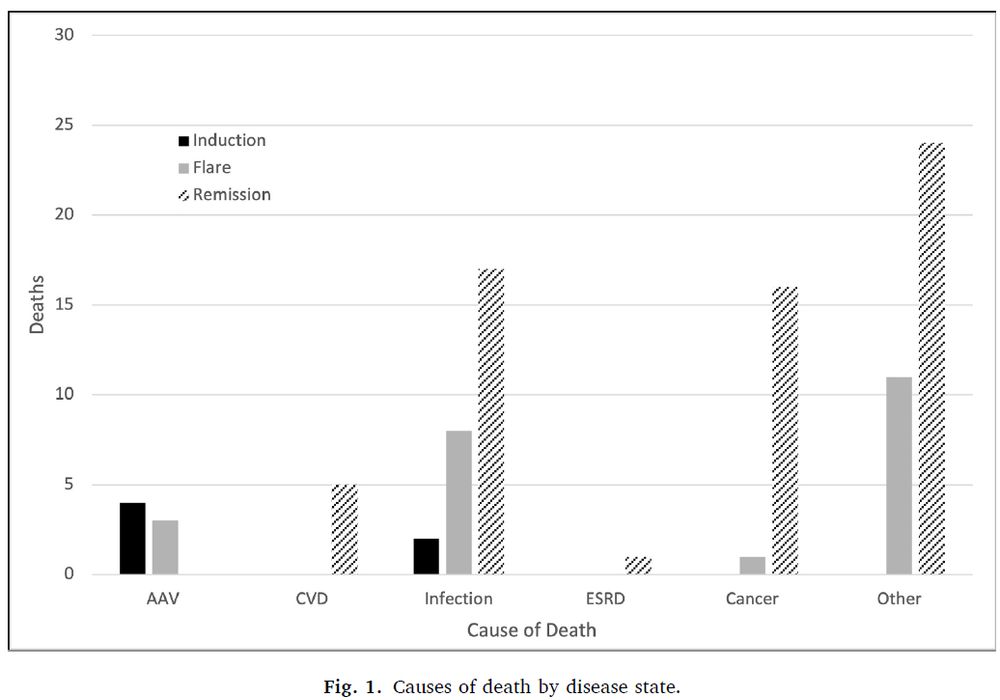




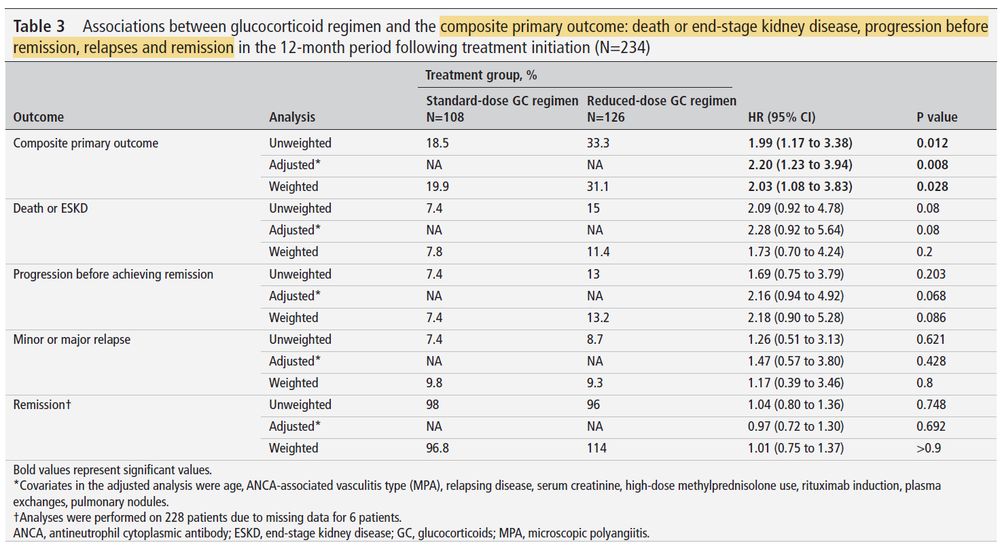
▶️ higher number of relapse at 6 months for the discontinuation group
▶️ but driven by minor relapses and by subgroup not treated but Rituximab.
Presented by Pr. Peter Merkel #ACR24 (acrabstracts.org/abstract/a-m...)
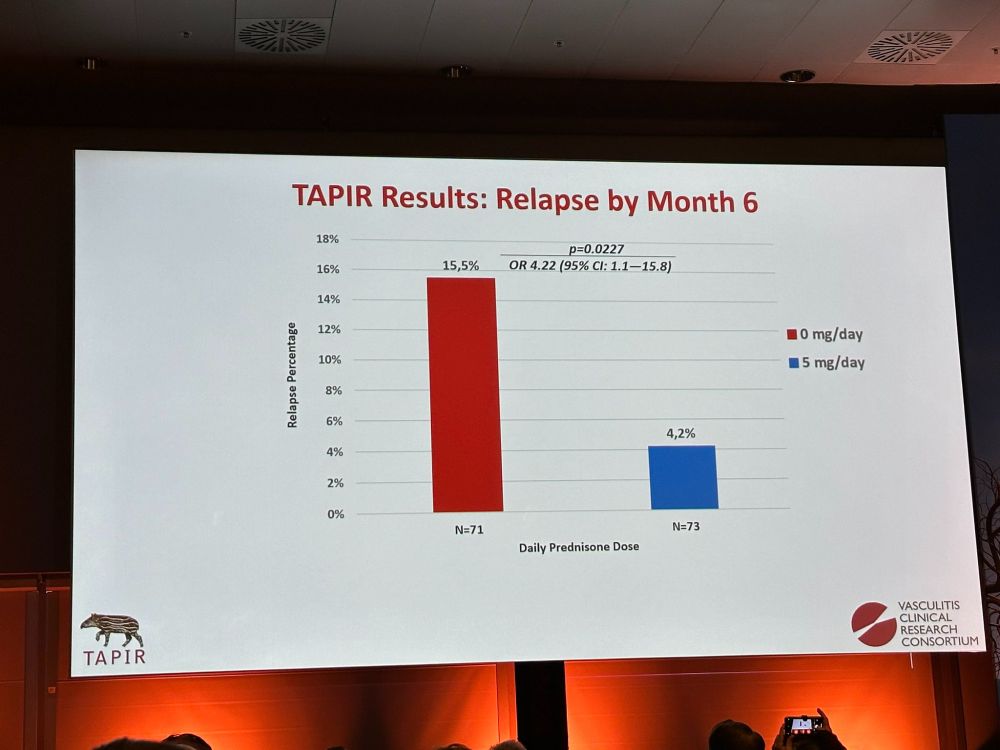
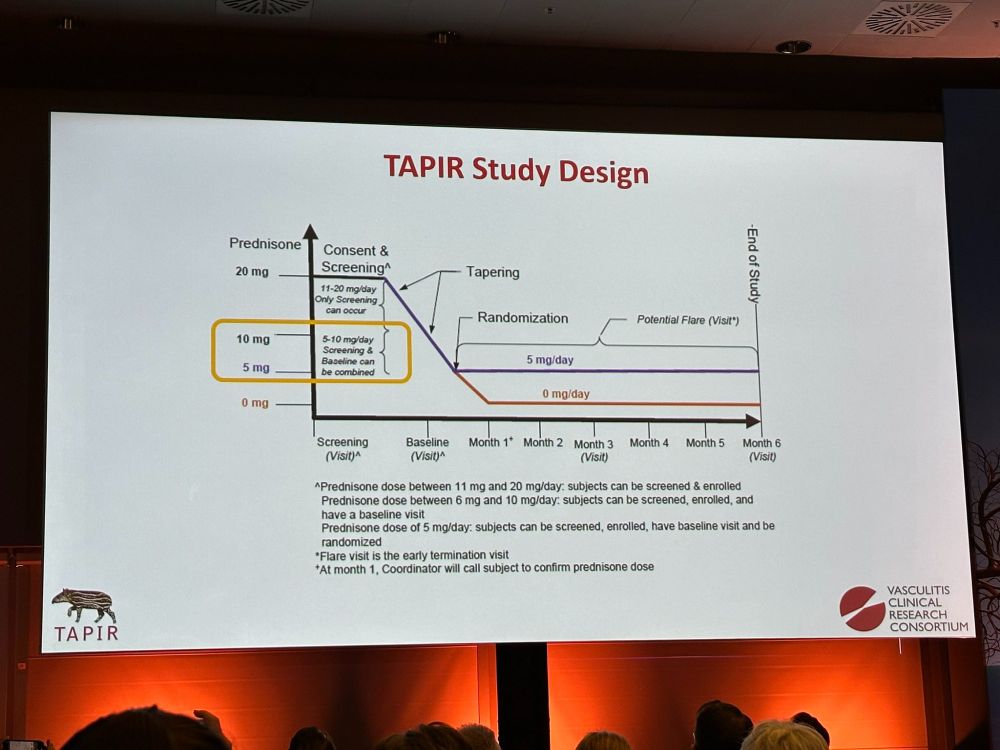
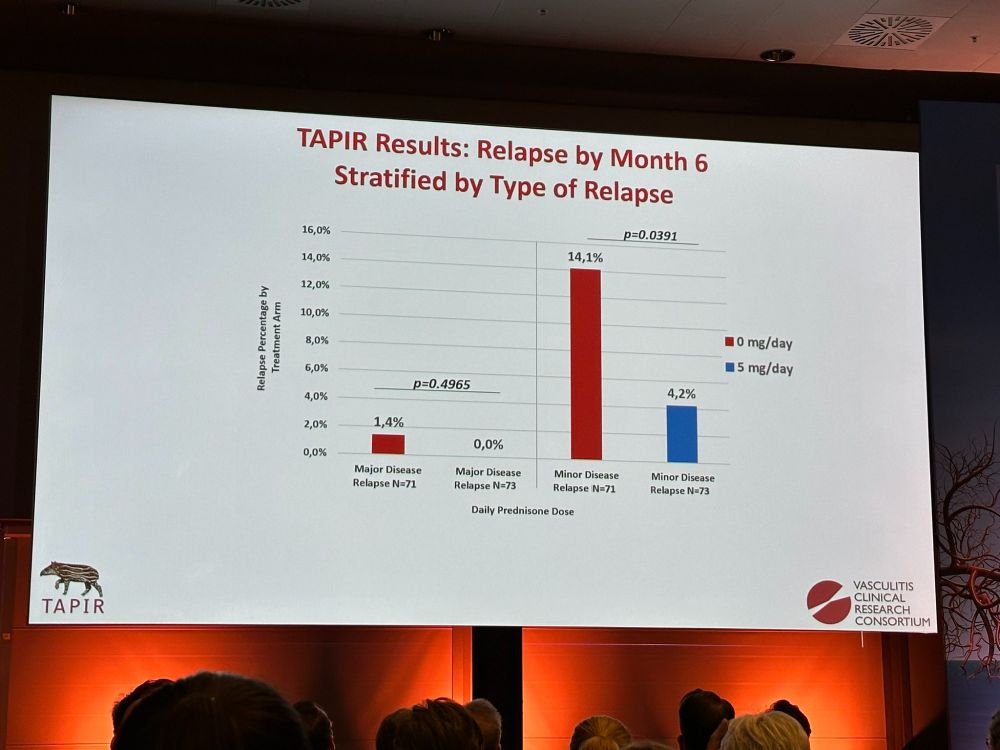
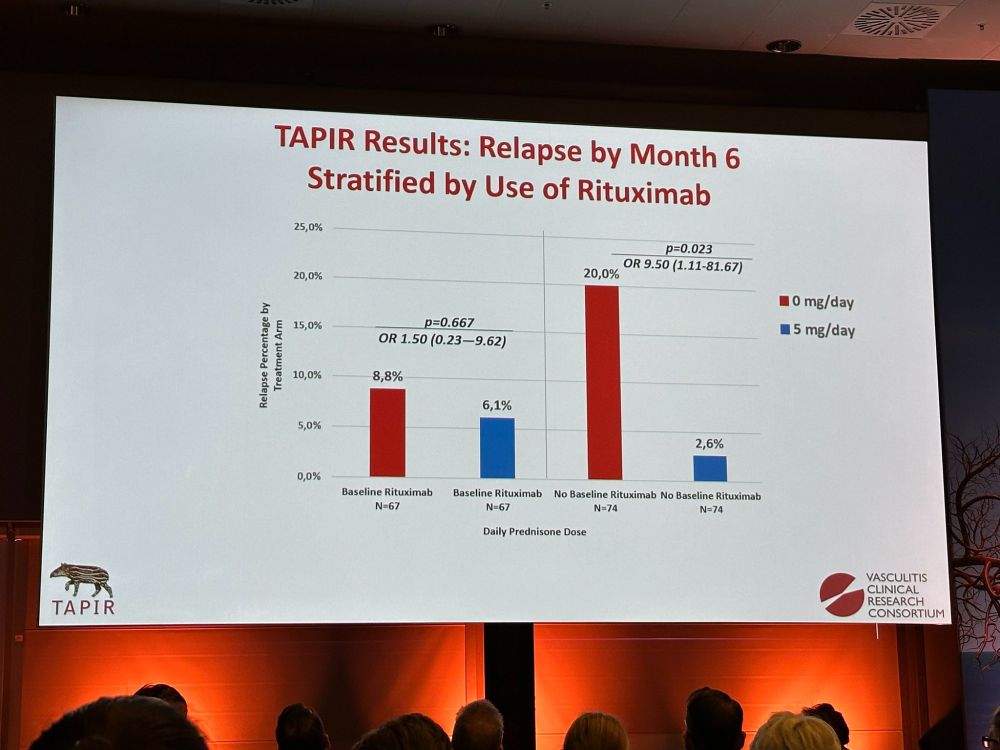
▶️ higher number of relapse at 6 months for the discontinuation group
▶️ but driven by minor relapses and by subgroup not treated but Rituximab.
Presented by Pr. Peter Merkel #ACR24 (acrabstracts.org/abstract/a-m...)