
Stanford Antimicrobial Safety & Sustainability Program
@stanfordasp.bsky.social
🏆 IDSA Center of Excellence in Antimicrobial Stewardship | CDPH AMS Honor Roll Gold | WHO Collaborating Centre
🩺 Stan Deresinski, Marisa Holubar, Alex Zimmet, Amy Chang, Emily Mui, Lina Meng, Will Alegria, David Ha
🔗 http://med.stanford.edu/bugsanddrugs
🩺 Stan Deresinski, Marisa Holubar, Alex Zimmet, Amy Chang, Emily Mui, Lina Meng, Will Alegria, David Ha
🔗 http://med.stanford.edu/bugsanddrugs
For more on our institution's SHC Pneumonia Guidelines, check the figure and link below! 🔗https://med.stanford.edu/bugsanddrugs/guidebook.html#pulmonary

October 29, 2025 at 7:07 PM
For more on our institution's SHC Pneumonia Guidelines, check the figure and link below! 🔗https://med.stanford.edu/bugsanddrugs/guidebook.html#pulmonary
📊 See the figure below to review antifungal coverage.

September 17, 2025 at 5:08 PM
📊 See the figure below to review antifungal coverage.
See figure for MRSA and PsA Risk factors in CAP from Stanford.
💊 If your patient lacks these risk factors, consider CAP treatment with ceftriaxone and azithromycin.
💊 If your patient lacks these risk factors, consider CAP treatment with ceftriaxone and azithromycin.

September 10, 2025 at 5:32 PM
See figure for MRSA and PsA Risk factors in CAP from Stanford.
💊 If your patient lacks these risk factors, consider CAP treatment with ceftriaxone and azithromycin.
💊 If your patient lacks these risk factors, consider CAP treatment with ceftriaxone and azithromycin.
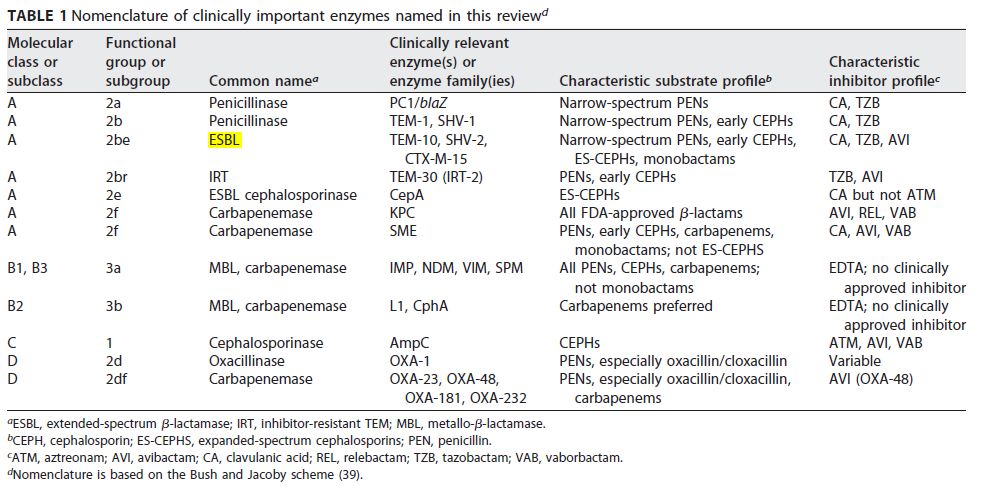
For the micro nerd:
Important beta-lactamases & nomenclature is shown in this table by Bush et al. Great review article here: pubmed.ncbi.nlm.nih.gov/32102899/
Important beta-lactamases & nomenclature is shown in this table by Bush et al. Great review article here: pubmed.ncbi.nlm.nih.gov/32102899/
August 6, 2025 at 4:45 PM
For the micro nerd:
Important beta-lactamases & nomenclature is shown in this table by Bush et al. Great review article here: pubmed.ncbi.nlm.nih.gov/32102899/
Important beta-lactamases & nomenclature is shown in this table by Bush et al. Great review article here: pubmed.ncbi.nlm.nih.gov/32102899/
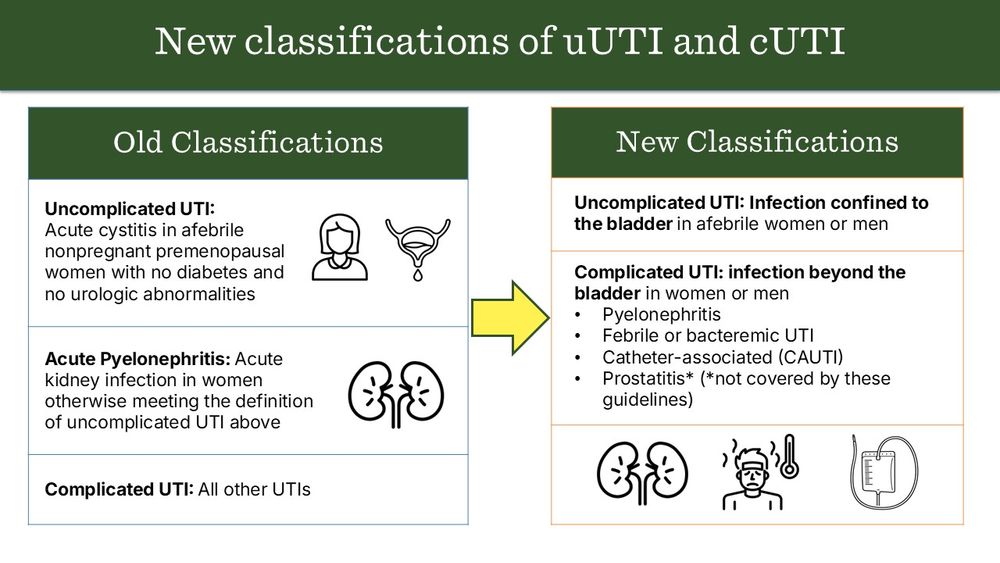
💡 A: No, he does not have a complicated UTI. While it was previously thought that male gender, anatomic abnormalities, or immunocompromised status always indicated a complicated UTI, this is no longer supported by IDSA guidelines.(1,2) See Classification of UTI here:
July 24, 2025 at 2:52 PM
💡 A: No, he does not have a complicated UTI. While it was previously thought that male gender, anatomic abnormalities, or immunocompromised status always indicated a complicated UTI, this is no longer supported by IDSA guidelines.(1,2) See Classification of UTI here:
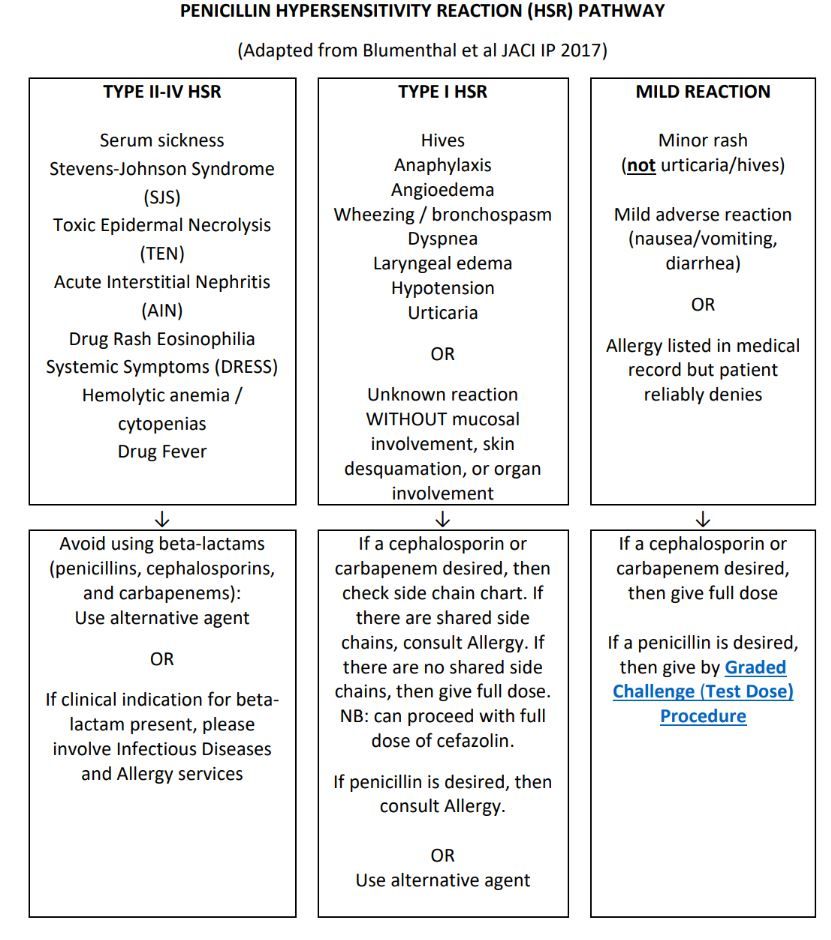
📊 Check out our PCN allergy algorithm for more guidance!
(Note, ceph allergy algorithm not shown here)
(Note, ceph allergy algorithm not shown here)
July 16, 2025 at 3:23 PM
📊 Check out our PCN allergy algorithm for more guidance!
(Note, ceph allergy algorithm not shown here)
(Note, ceph allergy algorithm not shown here)
🔍 For a review of posaconazole’s spectrum of activity, see the attached figure. PMID: 21803962
⚠️ If there is ever concern for breakthrough infection, it’s best to consult Infectious Diseases (ID).
⚠️ If there is ever concern for breakthrough infection, it’s best to consult Infectious Diseases (ID).

June 11, 2025 at 2:21 PM
🔍 For a review of posaconazole’s spectrum of activity, see the attached figure. PMID: 21803962
⚠️ If there is ever concern for breakthrough infection, it’s best to consult Infectious Diseases (ID).
⚠️ If there is ever concern for breakthrough infection, it’s best to consult Infectious Diseases (ID).
3️⃣ Switching to 2nd-line prophylactic agents, e.g. atovaquone & dapsone are LESS EFFECTIVE than TMP/SMX at preventing PJP and opportunistic infections caused by Listeria monocytogenes, Toxoplasma gondii, and Nocardia spp. & can lead to breakthrough infections and significant morbidity and mortality.

June 4, 2025 at 2:13 PM
3️⃣ Switching to 2nd-line prophylactic agents, e.g. atovaquone & dapsone are LESS EFFECTIVE than TMP/SMX at preventing PJP and opportunistic infections caused by Listeria monocytogenes, Toxoplasma gondii, and Nocardia spp. & can lead to breakthrough infections and significant morbidity and mortality.
🔍 If enterococcal coverage is desired (see risk factors), note that vancomycin does not add much if you are already using piperacillin/tazobactam, as it covers E. faecalis. Remember, E. faecium is usually vancomycin-resistant (VRE).

May 14, 2025 at 4:42 PM
🔍 If enterococcal coverage is desired (see risk factors), note that vancomycin does not add much if you are already using piperacillin/tazobactam, as it covers E. faecalis. Remember, E. faecium is usually vancomycin-resistant (VRE).
⚠️ If used in hospitalized patients with underlying heart conditions or multiple risk factors, use with caution and closely monitor QTc. The risk of QTc prolongation is LOWEST with CIPROFLOXACIN. See figure for comparison between FQs.

April 24, 2025 at 2:36 PM
⚠️ If used in hospitalized patients with underlying heart conditions or multiple risk factors, use with caution and closely monitor QTc. The risk of QTc prolongation is LOWEST with CIPROFLOXACIN. See figure for comparison between FQs.
🔄 Transition to PO (e.g. cipro, TMP-SMX) when able!
📊 Recent data supports the use of shorter courses (3 days) for treatment (PMID: 35467310), though this has not yet been incorporated into the guidelines. Check out our local IAI guidelines. med.stanford.edu/content/dam/...
📊 Recent data supports the use of shorter courses (3 days) for treatment (PMID: 35467310), though this has not yet been incorporated into the guidelines. Check out our local IAI guidelines. med.stanford.edu/content/dam/...

December 10, 2024 at 8:55 PM
🔄 Transition to PO (e.g. cipro, TMP-SMX) when able!
📊 Recent data supports the use of shorter courses (3 days) for treatment (PMID: 35467310), though this has not yet been incorporated into the guidelines. Check out our local IAI guidelines. med.stanford.edu/content/dam/...
📊 Recent data supports the use of shorter courses (3 days) for treatment (PMID: 35467310), though this has not yet been incorporated into the guidelines. Check out our local IAI guidelines. med.stanford.edu/content/dam/...
⚠️ Different Strep species have varying "stickiness." Risk is highest with:
Viridans group streptococci and Strep gallolyticus (bovis) - IE prevalence 35.7%
Low-risk with S. pneumoniae, S. pyogenes, and S. intermedius - IE prevalence 0.5–6.9%
(Chamat-Hedemand et al Circulation 2020)
Viridans group streptococci and Strep gallolyticus (bovis) - IE prevalence 35.7%
Low-risk with S. pneumoniae, S. pyogenes, and S. intermedius - IE prevalence 0.5–6.9%
(Chamat-Hedemand et al Circulation 2020)

December 4, 2024 at 6:21 PM
⚠️ Different Strep species have varying "stickiness." Risk is highest with:
Viridans group streptococci and Strep gallolyticus (bovis) - IE prevalence 35.7%
Low-risk with S. pneumoniae, S. pyogenes, and S. intermedius - IE prevalence 0.5–6.9%
(Chamat-Hedemand et al Circulation 2020)
Viridans group streptococci and Strep gallolyticus (bovis) - IE prevalence 35.7%
Low-risk with S. pneumoniae, S. pyogenes, and S. intermedius - IE prevalence 0.5–6.9%
(Chamat-Hedemand et al Circulation 2020)
🔗 See SHC UTI ABX Guidelines for tx options for ESBL cystitis.
🔍 One approach under investigation is to combine amoxicillin/clavulanate with certain oral cephalosporins (e.g., cefixime) for ESBL E. coli cystitis. More clinical data is needed on this strategy! (see PMID: 31107146, 30117050)
🔍 One approach under investigation is to combine amoxicillin/clavulanate with certain oral cephalosporins (e.g., cefixime) for ESBL E. coli cystitis. More clinical data is needed on this strategy! (see PMID: 31107146, 30117050)

December 3, 2024 at 9:31 PM
🔗 See SHC UTI ABX Guidelines for tx options for ESBL cystitis.
🔍 One approach under investigation is to combine amoxicillin/clavulanate with certain oral cephalosporins (e.g., cefixime) for ESBL E. coli cystitis. More clinical data is needed on this strategy! (see PMID: 31107146, 30117050)
🔍 One approach under investigation is to combine amoxicillin/clavulanate with certain oral cephalosporins (e.g., cefixime) for ESBL E. coli cystitis. More clinical data is needed on this strategy! (see PMID: 31107146, 30117050)
🌟 ABX Pearl of the Day: AmpC or ESBL?
📋 Q: How can I quickly spot the difference in AmpC and ESBL resistance patterns? 🤔
🩺 A: Step 1: Look at the organism. Step 2: Check ceftriaxone susceptibility. Here’s a quick & handy decision tree to inform ABX Rx 👇 #IDsky #MedSky #PharmSky
🔗 IDSA AMR Guidance
📋 Q: How can I quickly spot the difference in AmpC and ESBL resistance patterns? 🤔
🩺 A: Step 1: Look at the organism. Step 2: Check ceftriaxone susceptibility. Here’s a quick & handy decision tree to inform ABX Rx 👇 #IDsky #MedSky #PharmSky
🔗 IDSA AMR Guidance

November 25, 2024 at 7:37 PM
🌟 ABX Pearl of the Day: Duration of treatment in intra-abdominal infections (IAI)! 💊
💡 Q: How long should I treat IAI after source control?
🔍 A: While STOP-IT trial calls for 4 days post-source control, there are notable exceptions. See infographic for details 👇
#IDsky #AMSsky #MedSky #Pharmsky
💡 Q: How long should I treat IAI after source control?
🔍 A: While STOP-IT trial calls for 4 days post-source control, there are notable exceptions. See infographic for details 👇
#IDsky #AMSsky #MedSky #Pharmsky

November 22, 2024 at 6:07 PM
✅ A: To minimize C. diff infection risk:
1️⃣ Limit cumulative antibiotic exposure.
2️⃣ Use the narrowest spectrum antibiotic for the shortest duration needed for the infection.
🧐 Click to see which ABX are most frequently associated with hospital-associated CDI. (PMID: 31964789)
1️⃣ Limit cumulative antibiotic exposure.
2️⃣ Use the narrowest spectrum antibiotic for the shortest duration needed for the infection.
🧐 Click to see which ABX are most frequently associated with hospital-associated CDI. (PMID: 31964789)

November 21, 2024 at 5:12 PM
✅ A: To minimize C. diff infection risk:
1️⃣ Limit cumulative antibiotic exposure.
2️⃣ Use the narrowest spectrum antibiotic for the shortest duration needed for the infection.
🧐 Click to see which ABX are most frequently associated with hospital-associated CDI. (PMID: 31964789)
1️⃣ Limit cumulative antibiotic exposure.
2️⃣ Use the narrowest spectrum antibiotic for the shortest duration needed for the infection.
🧐 Click to see which ABX are most frequently associated with hospital-associated CDI. (PMID: 31964789)
🔍 A: Let’s distinguish between aspiration pneumonitis and aspiration pneumonia. Both can present with fever, tachycardia, hypoxia, cough, leukocytosis, and elevated PCT. See image below for key 🗝️ differences.

November 18, 2024 at 6:44 PM
🔍 A: Let’s distinguish between aspiration pneumonitis and aspiration pneumonia. Both can present with fever, tachycardia, hypoxia, cough, leukocytosis, and elevated PCT. See image below for key 🗝️ differences.
Q: How long do I treat for UTI?
A: Please see updated definitions (2024) of uncomplicated vs complicated UTI and corresponding treatment durations in this infographic.
A: Please see updated definitions (2024) of uncomplicated vs complicated UTI and corresponding treatment durations in this infographic.

November 13, 2024 at 10:01 PM
Q: How long do I treat for UTI?
A: Please see updated definitions (2024) of uncomplicated vs complicated UTI and corresponding treatment durations in this infographic.
A: Please see updated definitions (2024) of uncomplicated vs complicated UTI and corresponding treatment durations in this infographic.


