
The gut–brain–immune axis can shape how symptoms show up—especially when GI problems are in the mix.
Here’s what clinicians needs to know about Gut Microbiome and Autism Spectrum Disorder (ASD) 👇🧵

The gut–brain–immune axis can shape how symptoms show up—especially when GI problems are in the mix.
Here’s what clinicians needs to know about Gut Microbiome and Autism Spectrum Disorder (ASD) 👇🧵




This diagnostic tool detects a patient’s latent anxiety.
These items are answered by frequency (not at all, most days, etc.)
[Spitzer et al., 2006]
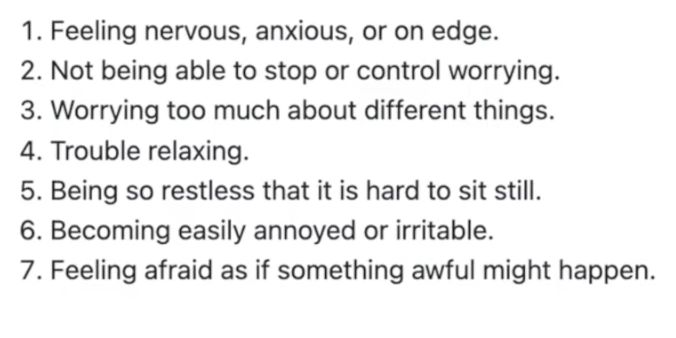
This diagnostic tool detects a patient’s latent anxiety.
These items are answered by frequency (not at all, most days, etc.)
[Spitzer et al., 2006]
Excessive worry more days than not for ≥6 months about multiple domains, difficult to control.
Plus ≥3 of restlessness, fatigue, poor concentration/mind blank, irritability, muscle tension, and sleep disturbance.

Excessive worry more days than not for ≥6 months about multiple domains, difficult to control.
Plus ≥3 of restlessness, fatigue, poor concentration/mind blank, irritability, muscle tension, and sleep disturbance.
Onset with VCE exams; now pervasive worry, decision paralysis, and no depressive features.
You suspect GAD.
What would you do to confirm this? 👇

Onset with VCE exams; now pervasive worry, decision paralysis, and no depressive features.
You suspect GAD.
What would you do to confirm this? 👇
Research shows a significant male-to-female diagnosis gap (Berry et al., 1985).
Let’s explore why ADHD presents differently in females.

Research shows a significant male-to-female diagnosis gap (Berry et al., 1985).
Let’s explore why ADHD presents differently in females.
Research shows a significant male-to-female diagnosis gap (Berry et al., 1985).
Let’s explore why ADHD presents differently in females.

Research shows a significant male-to-female diagnosis gap (Berry et al., 1985).
Let’s explore why ADHD presents differently in females.
Miss one, and you may miss risk.
Here’s what to look for and how to act 👇🧵

Miss one, and you may miss risk.
Here’s what to look for and how to act 👇🧵
Miss one, and you may miss risk.
Here’s what to look for and how to act 👇🧵

Miss one, and you may miss risk.
Here’s what to look for and how to act 👇🧵
Join Dr Sanil Rege for the ADHD Masterclass: From Neurobiology to Clinical Practice on the 29th of November:
https://learn.psychscene.com/adhdmasterclasslive

Join Dr Sanil Rege for the ADHD Masterclass: From Neurobiology to Clinical Practice on the 29th of November:
https://learn.psychscene.com/adhdmasterclasslive
Bottom-up circuits respond to salience: movement, novelty, reward.
In ADHD, underactive prefrontal regulation means bottom-up inputs (e.g. phone alerts, noise) more easily capture attention.

Bottom-up circuits respond to salience: movement, novelty, reward.
In ADHD, underactive prefrontal regulation means bottom-up inputs (e.g. phone alerts, noise) more easily capture attention.
When this system falters, stimulus-driven (“bottom-up”) networks dominate, explaining distractibility and inconsistent attention in ADHD.

When this system falters, stimulus-driven (“bottom-up”) networks dominate, explaining distractibility and inconsistent attention in ADHD.
It’s impaired prefrontal regulation across distributed circuits that shape attention, inhibition, and emotion.
Here’s how these circuits interact and what clinicians need to know about the neurobiology behind ADHD 🧵👇

It’s impaired prefrontal regulation across distributed circuits that shape attention, inhibition, and emotion.
Here’s how these circuits interact and what clinicians need to know about the neurobiology behind ADHD 🧵👇
https://psychscene.co/4nIEfTu

https://psychscene.co/4nIEfTu
Oestrogen delays onset in women—but symptoms surge after menopause.
Here’s how hormones shape outcomes + guide care. 👇🧵

Oestrogen delays onset in women—but symptoms surge after menopause.
Here’s how hormones shape outcomes + guide care. 👇🧵

Check out our evidence-based course, “PTSD & Complex PTSD: Advanced Clinical Training for Psychiatrists & Clinicians” on The Academy:
https://psychscene.co/4niwl3s

Check out our evidence-based course, “PTSD & Complex PTSD: Advanced Clinical Training for Psychiatrists & Clinicians” on The Academy:
https://psychscene.co/4niwl3s
Amygdala → acute fear.
BNST → sustained anxiety.
Hippocampal dysfunction → poor trauma contextualisation.
Dissociation disrupts these networks, leaving patients stuck in hyperarousal or shutdown.

Amygdala → acute fear.
BNST → sustained anxiety.
Hippocampal dysfunction → poor trauma contextualisation.
Dissociation disrupts these networks, leaving patients stuck in hyperarousal or shutdown.
🔹 Excess inhibition of the amygdala by the medial prefrontal cortex.
🔹 Over-regulation of fear → emotional numbing, detachment.
Psych Scene Tip: therapies that restore limbic-prefrontal balance (e.g., somatic and trauma-focused approaches) can help.

🔹 Excess inhibition of the amygdala by the medial prefrontal cortex.
🔹 Over-regulation of fear → emotional numbing, detachment.
Psych Scene Tip: therapies that restore limbic-prefrontal balance (e.g., somatic and trauma-focused approaches) can help.
Freeze → Flight → Fight → Fright → Flag → Faint.
Dissociation arises in fright/flag/faint when parasympathetic dominance triggers shutdown, immobility, and numbing.
Tracking shifts in arousal helps clinicians intervene.

Freeze → Flight → Fight → Fright → Flag → Faint.
Dissociation arises in fright/flag/faint when parasympathetic dominance triggers shutdown, immobility, and numbing.
Tracking shifts in arousal helps clinicians intervene.
1️⃣ Emotional undermodulation → hyperarousal, re-experiencing.
2️⃣ Emotional overmodulation → numbing, detachment, dissociation.
Understanding these helps match interventions:
- grounding for hyperarousal
- stabilisation before trauma processing in dissociation.

1️⃣ Emotional undermodulation → hyperarousal, re-experiencing.
2️⃣ Emotional overmodulation → numbing, detachment, dissociation.
Understanding these helps match interventions:
- grounding for hyperarousal
- stabilisation before trauma processing in dissociation.
Around 15–30% of patients with PTSD experience dissociative symptoms such as depersonalisation or derealisation.
Let’s discover why recognising dissociation is critical for tailoring therapy and improving outcomes. 👇🧵

Around 15–30% of patients with PTSD experience dissociative symptoms such as depersonalisation or derealisation.
Let’s discover why recognising dissociation is critical for tailoring therapy and improving outcomes. 👇🧵

