In this piece, myself and Charlotte Gupta (notoriously grounded individuals 👀 ) discuss the science behind grounding.
Link below 👇

In this piece, myself and Charlotte Gupta (notoriously grounded individuals 👀 ) discuss the science behind grounding.
Link below 👇
Excited to share our latest paper led by Dr. Matthew Morrison!
journals.humankinetics.com/view/journal...
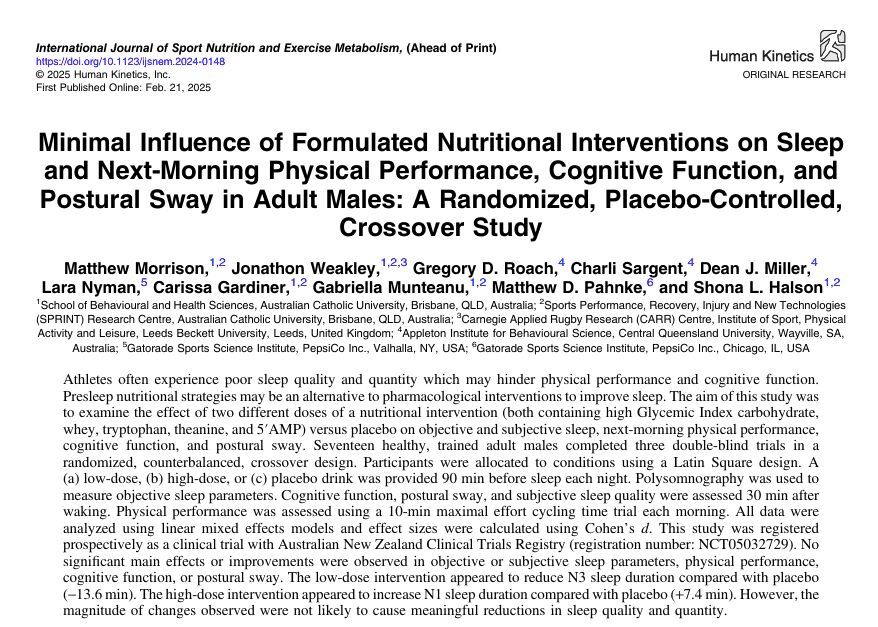
Excited to share our latest paper led by Dr. Matthew Morrison!
journals.humankinetics.com/view/journal...
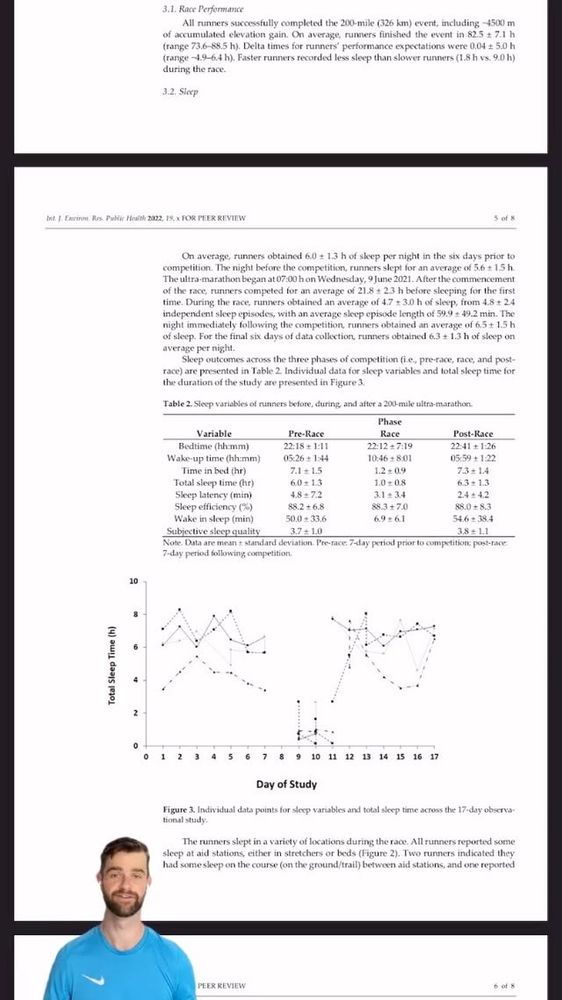
Find out the most common approaches to sleep during ultra-marathons, and our thoughts on future strategies in our open access paper.
mdpi.com/1720578
@academic-chatter.bsky.social @phdvoice.bsky.social
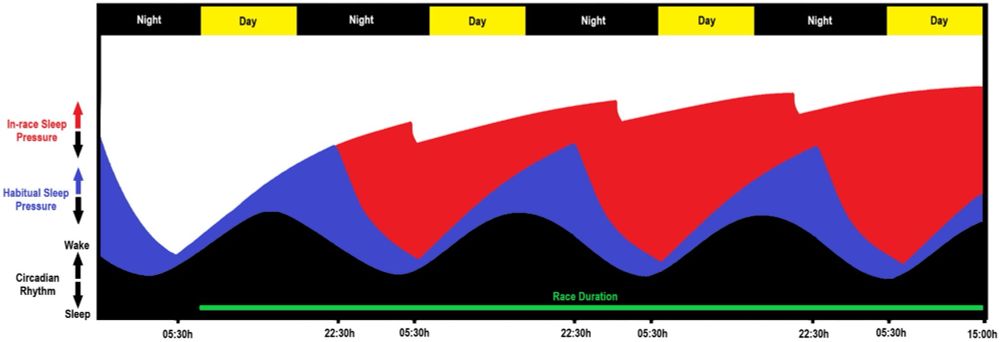
Find out the most common approaches to sleep during ultra-marathons, and our thoughts on future strategies in our open access paper.
mdpi.com/1720578
@academic-chatter.bsky.social @phdvoice.bsky.social
doi.org/10.3390/s221...
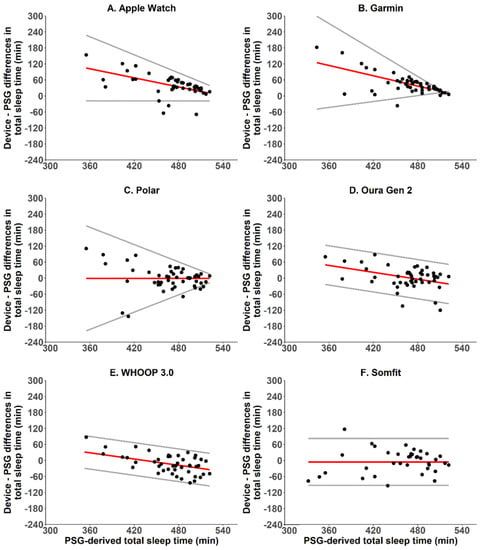
doi.org/10.3390/s221...
shorturl.at/RHOMB
shorturl.at/RHOMB
Have you ever noticed how alcohol impacts your sleep?
Our new paper, led by Dr Carissa Gardiner is now available as an online pre proof.
#sleep #sleepscience #alcohol
www.sciencedirect.com/science/arti...

Have you ever noticed how alcohol impacts your sleep?
Our new paper, led by Dr Carissa Gardiner is now available as an online pre proof.
#sleep #sleepscience #alcohol
www.sciencedirect.com/science/arti...
Find out the most common approaches to sleep during ultra-marathons, and our thoughts on future strategies in our new open access paper.
@darren__bianchi @sleeppsyc
mdpi.com/1720578

Find out the most common approaches to sleep during ultra-marathons, and our thoughts on future strategies in our new open access paper.
@darren__bianchi @sleeppsyc
mdpi.com/1720578
x.com/msprajcer/stat… doi.org/10.3390/ijerph…

x.com/msprajcer/stat… doi.org/10.3390/ijerph…
Chrononutrition Masterclass from @cc_gupta today at the @Sleep4Perform conference. Also heard from FMRS guru @msprajcer, with @ashmontero_ & @SSHRoberts to come in the evening session. Tune in if you can! #sleepscience

Chrononutrition Masterclass from @cc_gupta today at the @Sleep4Perform conference. Also heard from FMRS guru @msprajcer, with @ashmontero_ & @SSHRoberts to come in the evening session. Tune in if you can! #sleepscience
instagram.com/reel/CayZWnMA4… mdpi.com/1660-4601/19/5…

instagram.com/reel/CayZWnMA4… mdpi.com/1660-4601/19/5…
Acquiring a daily circadian biomarker with athletes in the field was challenging and enjoyable!
OPEN ACCESS
mdpi.com/2076-3417/11/2…

Acquiring a daily circadian biomarker with athletes in the field was challenging and enjoyable!
OPEN ACCESS
mdpi.com/2076-3417/11/2…
We examined the😴 of fit young males in no exercise 🛋️, aerobic exercise 🚴♂️, & resistance exercise 🏋️conditions (🛑@ 21:30)
Body temp⬆️after🚴♂️but returned to baseline before bedtime. Sleep did not differ across conditions.
FREE ACCESS:
x.com/EurJSportSci/s…
We examined the😴 of fit young males in no exercise 🛋️, aerobic exercise 🚴♂️, & resistance exercise 🏋️conditions (🛑@ 21:30)
Body temp⬆️after🚴♂️but returned to baseline before bedtime. Sleep did not differ across conditions.
FREE ACCESS:
x.com/EurJSportSci/s…
@AcademicChatter
x.com/SciMed_Footbal…
@AcademicChatter
x.com/SciMed_Footbal…

New paper in PLOS ONE:
x.com/drdeanjmiller/… doi.org/10.1371/journa…
Our new paper, in collaboration with @whoop, looks at changes in health promoting behaviour during physical distancing restrictions.
OPEN ACCESS link below:
dx.plos.org/10.1371/journa…
New paper in PLOS ONE:
x.com/drdeanjmiller/… doi.org/10.1371/journa…
Our new paper, in collaboration with @whoop, looks at changes in health promoting behaviour during physical distancing restrictions.
OPEN ACCESS link below:
dx.plos.org/10.1371/journa…
Our new paper, in collaboration with @whoop, looks at changes in health promoting behaviour during physical distancing restrictions.
OPEN ACCESS link below:
dx.plos.org/10.1371/journa…
x.com/drdeanjmiller/…
📉Drop in HR is start of question time🙋♀️

x.com/drdeanjmiller/…
📉Drop in HR is start of question time🙋♀️

📉Drop in HR is start of question time🙋♀️


Alcohol and gambling problems appear to be linked to insomnia 🥱
+ gambling problems may lead to poorer subjective sleep quality 💤
Read more below ⬇️
Great work from @gamblinghannah et al.
mdpi.com/1660-4601/18/1…

Alcohol and gambling problems appear to be linked to insomnia 🥱
+ gambling problems may lead to poorer subjective sleep quality 💤
Read more below ⬇️
Great work from @gamblinghannah et al.
mdpi.com/1660-4601/18/1…
The Relationship Between Diet and Sleep in Older Adults: a Narrative Review 🍒🥛@AcademicChatter #SleepPeeps
x.com/cc_gupta/statu… link.springer.com/article/10.100…
The Relationship Between Diet and Sleep in Older Adults: a Narrative Review 🍒🥛@AcademicChatter #SleepPeeps
x.com/cc_gupta/statu… link.springer.com/article/10.100…