This work shows how quantitative EEG markers can help clarify what makes IH distinct.
🧵Thanks for reading!
📄 Read the preprint here: www.biorxiv.org/content/10.1...
🔁 Questions, and feedback welcome!

This work shows how quantitative EEG markers can help clarify what makes IH distinct.
🧵Thanks for reading!
📄 Read the preprint here: www.biorxiv.org/content/10.1...
🔁 Questions, and feedback welcome!
IH with long sleep time isn’t marked by “bad sleep” but by paradoxically deep and structured sleep, paired with excessive daytime sleepiness.
⏰ It’s time to look beyond the night
→ into daytime arousal systems and brain function during wakefulness.

IH with long sleep time isn’t marked by “bad sleep” but by paradoxically deep and structured sleep, paired with excessive daytime sleepiness.
⏰ It’s time to look beyond the night
→ into daytime arousal systems and brain function during wakefulness.
Using just one night of EEG, our model classified IH vs. controls with an AUC of 0.74 🎯
Still far from perfect, but it’s a step toward more objective, EEG-based diagnostics.

Using just one night of EEG, our model classified IH vs. controls with an AUC of 0.74 🎯
Still far from perfect, but it’s a step toward more objective, EEG-based diagnostics.
Slow waves are linked to sleep inertia, and may reflect heightened sleep pressure.
Two (non-exclusive) hypotheses:
🧠 Increased synaptic plasticity during wake
🔥 Altered brain metabolism
Either way → sleep may be normal, but wake is off.
Slow waves are linked to sleep inertia, and may reflect heightened sleep pressure.
Two (non-exclusive) hypotheses:
🧠 Increased synaptic plasticity during wake
🔥 Altered brain metabolism
Either way → sleep may be normal, but wake is off.
💡 IH patients showed increased slow wave density during N3 despite no change in overall delta power.
This implies that global spectral analyses may miss subtle but meaningful changes in sleep microarchitecture.

💡 IH patients showed increased slow wave density during N3 despite no change in overall delta power.
This implies that global spectral analyses may miss subtle but meaningful changes in sleep microarchitecture.
📉 suggesting that while local sleep dynamics are altered, global regulatory rhythms (like those influenced by noradrenaline) may stay intact.

📉 suggesting that while local sleep dynamics are altered, global regulatory rhythms (like those influenced by noradrenaline) may stay intact.
📈 IH patients had more sigma power & higher spindle density
🧠 Spindles were more clustered, pointing to over-stabilized thalamocortical networks
→ This might underlie severe sleep inertia and reduced responsiveness to stimuli.

📈 IH patients had more sigma power & higher spindle density
🧠 Spindles were more clustered, pointing to over-stabilized thalamocortical networks
→ This might underlie severe sleep inertia and reduced responsiveness to stimuli.
➡️ IH patients showed less similarity between consecutive NREM epochs.
Not due to awakenings or hybrid stages like insomnia (see thread : shorturl.at/QDlol) or NT1,
but perhaps a different kind of sleep instability 🤔
➡️ IH patients showed less similarity between consecutive NREM epochs.
Not due to awakenings or hybrid stages like insomnia (see thread : shorturl.at/QDlol) or NT1,
but perhaps a different kind of sleep instability 🤔
So, we turned to the analysis of hypnodensity 📊:
IH showed more mixed wake/N1 epochs, especially during intra-sleep awakenings.
⚠️ Are these a marker of sleep intrusions into wakefulness and difficulty fully waking up?
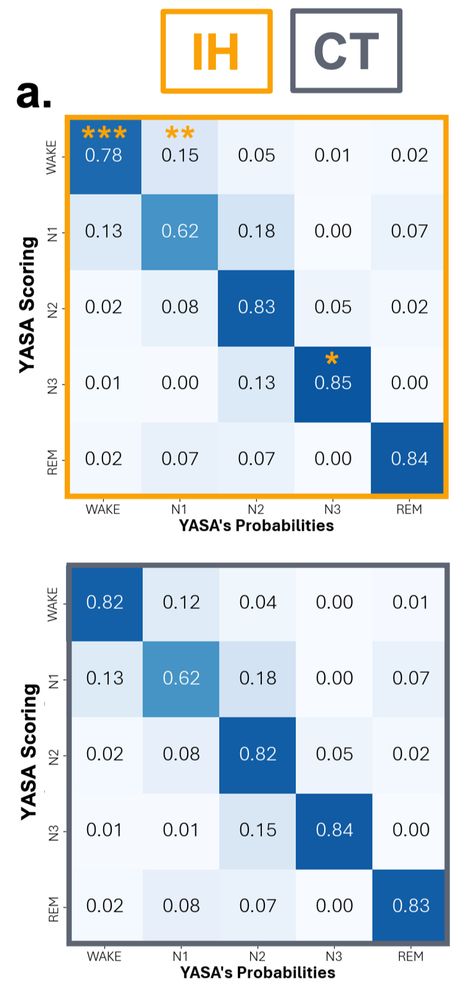
So, we turned to the analysis of hypnodensity 📊:
IH showed more mixed wake/N1 epochs, especially during intra-sleep awakenings.
⚠️ Are these a marker of sleep intrusions into wakefulness and difficulty fully waking up?
🛌 IH participants had more N3 and higher sleep efficiency
😴 Less REM and reduced wake after sleep onset
📉 These results might partly reflect the way sleep tests are run (e.g., waking at 6:30am for MSLT → less REM at the end of the night)

🛌 IH participants had more N3 and higher sleep efficiency
😴 Less REM and reduced wake after sleep onset
📉 These results might partly reflect the way sleep tests are run (e.g., waking at 6:30am for MSLT → less REM at the end of the night)
So we looked beyond classic metrics like REM %, sleep efficiency, or MSLT latency…
…and dove into sleep microarchitecture. 🧠💤

So we looked beyond classic metrics like REM %, sleep efficiency, or MSLT latency…
…and dove into sleep microarchitecture. 🧠💤

