Andrea Mazzella
@andmazzella.bsky.social
Public Health Medicine registrar (resident doctor), epidemiologist, migrant, geek in disguise.📍 London | 🗣️ an-DREH-ah | 👤 he/him
That's a wrap on #ESCMIDGlobal! I'm going to miss the Viennese bread.

April 15, 2025 at 8:19 PM
That's a wrap on #ESCMIDGlobal! I'm going to miss the Viennese bread.
Interesting #ESCMIDGlobal poster by @seanong.bsky.social showing how often ID trials do not report on key social factors. Which is absurd, as we know how important social determinants are for infectious diseases!

April 15, 2025 at 11:32 AM
Interesting #ESCMIDGlobal poster by @seanong.bsky.social showing how often ID trials do not report on key social factors. Which is absurd, as we know how important social determinants are for infectious diseases!
Great presentation by Prof Mike Sharland on global AMR policy
Excellent reminder that 90% of total antibiotic use is in the community, not in hospitals! Yet infection specialists seem focussed on the hospital setting
#escmidglobal #escmid2025
Excellent reminder that 90% of total antibiotic use is in the community, not in hospitals! Yet infection specialists seem focussed on the hospital setting
#escmidglobal #escmid2025

April 13, 2025 at 9:26 AM
Great presentation by Prof Mike Sharland on global AMR policy
Excellent reminder that 90% of total antibiotic use is in the community, not in hospitals! Yet infection specialists seem focussed on the hospital setting
#escmidglobal #escmid2025
Excellent reminder that 90% of total antibiotic use is in the community, not in hospitals! Yet infection specialists seem focussed on the hospital setting
#escmidglobal #escmid2025
@dianeashiru.bsky.social presenting at #ESCMID2025 on which indicators can be used to track use and appropriateness of antimicrobials
As always in surveillance there's a balance to strike between usefulness of results and burden of data collection. Proxy indicators helpful
As always in surveillance there's a balance to strike between usefulness of results and burden of data collection. Proxy indicators helpful

April 13, 2025 at 7:23 AM
@dianeashiru.bsky.social presenting at #ESCMID2025 on which indicators can be used to track use and appropriateness of antimicrobials
As always in surveillance there's a balance to strike between usefulness of results and burden of data collection. Proxy indicators helpful
As always in surveillance there's a balance to strike between usefulness of results and burden of data collection. Proxy indicators helpful
#ESCMID2025, today I'm presenting the results of national surveillance of bloodstream infections in critical care units in England.
Come say hi if you're interested in infections in critical care
Poster sector A, row 6, position 7
#EpiSky
Come say hi if you're interested in infections in critical care
Poster sector A, row 6, position 7
#EpiSky

April 13, 2025 at 6:54 AM
#ESCMID2025, today I'm presenting the results of national surveillance of bloodstream infections in critical care units in England.
Come say hi if you're interested in infections in critical care
Poster sector A, row 6, position 7
#EpiSky
Come say hi if you're interested in infections in critical care
Poster sector A, row 6, position 7
#EpiSky
When looking at ethnicity, the white group had the highest crude incidence of bacteraemia.
However, on average white people in England are older than the minority ethnic groups, so they already have a higher risk of bacteraemia.
Once we adjusted for age structure, we saw some interesting patterns.
However, on average white people in England are older than the minority ethnic groups, so they already have a higher risk of bacteraemia.
Once we adjusted for age structure, we saw some interesting patterns.

March 6, 2025 at 5:33 PM
When looking at ethnicity, the white group had the highest crude incidence of bacteraemia.
However, on average white people in England are older than the minority ethnic groups, so they already have a higher risk of bacteraemia.
Once we adjusted for age structure, we saw some interesting patterns.
However, on average white people in England are older than the minority ethnic groups, so they already have a higher risk of bacteraemia.
Once we adjusted for age structure, we saw some interesting patterns.
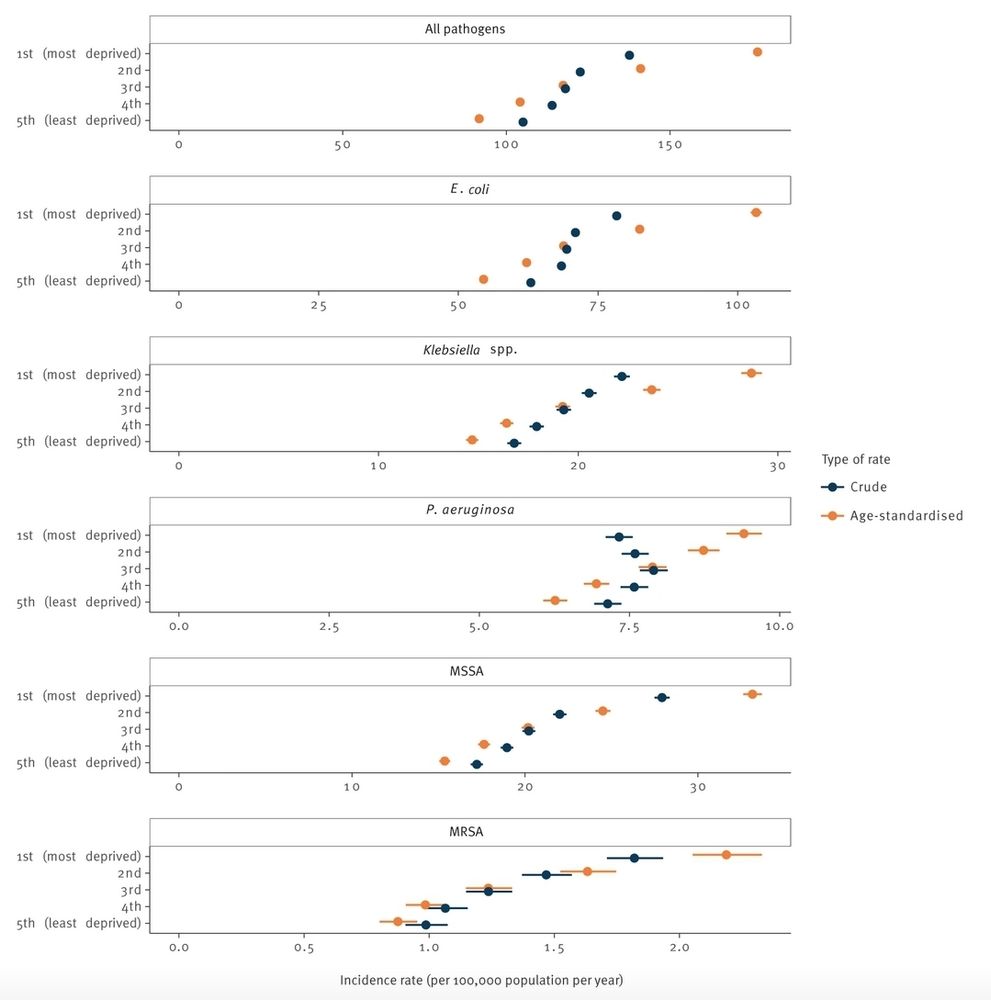
Unsurprisingly, the most deprived areas of the country had the highest incidence of these serious infections.
Once we adjusted for age, this health inequality was even more striking: the most deprived areas had double the rate of the least deprived areas (95% CI: 1.89–2.15).
Once we adjusted for age, this health inequality was even more striking: the most deprived areas had double the rate of the least deprived areas (95% CI: 1.89–2.15).
March 6, 2025 at 5:33 PM
Unsurprisingly, the most deprived areas of the country had the highest incidence of these serious infections.
Once we adjusted for age, this health inequality was even more striking: the most deprived areas had double the rate of the least deprived areas (95% CI: 1.89–2.15).
Once we adjusted for age, this health inequality was even more striking: the most deprived areas had double the rate of the least deprived areas (95% CI: 1.89–2.15).
The type of talks that infectious disease epidemiologists are invited to attend:

January 24, 2025 at 4:50 PM
The type of talks that infectious disease epidemiologists are invited to attend:
Interestingly, there was a *decreasing* trend of resistance in P. aeruginosa to ciprofloxacin and in E. coli to amoxicillin/clavulanate:
[🧵 8/9]
[🧵 8/9]

January 16, 2025 at 5:35 PM
Interestingly, there was a *decreasing* trend of resistance in P. aeruginosa to ciprofloxacin and in E. coli to amoxicillin/clavulanate:
[🧵 8/9]
[🧵 8/9]
And Enterobacter cloacae isolates from BSI became more commonly resistant to ceftazidime and piperacillin/tazobactam:
[🧵 7/9]
[🧵 7/9]

January 16, 2025 at 5:35 PM
And Enterobacter cloacae isolates from BSI became more commonly resistant to ceftazidime and piperacillin/tazobactam:
[🧵 7/9]
[🧵 7/9]
Some #AMR profiles changed during the years.
K. pneumoniae isolates from BSI became more commonly resistant to both amoxicillin/clavulanate and piperacillin/tazobactam:
[🧵 6/9]
K. pneumoniae isolates from BSI became more commonly resistant to both amoxicillin/clavulanate and piperacillin/tazobactam:
[🧵 6/9]

January 16, 2025 at 5:35 PM
Some #AMR profiles changed during the years.
K. pneumoniae isolates from BSI became more commonly resistant to both amoxicillin/clavulanate and piperacillin/tazobactam:
[🧵 6/9]
K. pneumoniae isolates from BSI became more commonly resistant to both amoxicillin/clavulanate and piperacillin/tazobactam:
[🧵 6/9]
Meanwhile, other common causes of BSI in CCUs such as Candida temporarly became less common.
[🧵 4/9]
[🧵 4/9]

January 16, 2025 at 5:35 PM
Meanwhile, other common causes of BSI in CCUs such as Candida temporarly became less common.
[🧵 4/9]
[🧵 4/9]
This peak in incidence was also associated to an increase of BSI caused by Enterococcus and Klebsiella species.
Maybe this was because of the changes in patient care, patient case-mix and again IPC practices.
[🧵 3/9]
Maybe this was because of the changes in patient care, patient case-mix and again IPC practices.
[🧵 3/9]

January 16, 2025 at 5:35 PM
This peak in incidence was also associated to an increase of BSI caused by Enterococcus and Klebsiella species.
Maybe this was because of the changes in patient care, patient case-mix and again IPC practices.
[🧵 3/9]
Maybe this was because of the changes in patient care, patient case-mix and again IPC practices.
[🧵 3/9]
My first discovery on BlueSky! Looking forward to digging in @zetkin.bsky.social @mkellyirving.bsky.social

November 20, 2024 at 8:39 PM
My first discovery on BlueSky! Looking forward to digging in @zetkin.bsky.social @mkellyirving.bsky.social



