Junqiang(John) Zhao
@junqiangzhao.bsky.social
Assist Prof University of rochester Medical center. Supprotive care in cancer #ImpSci #Shared_decision_making #Realist_methodology
Reposted by Junqiang(John) Zhao
Hi #impsci friends! Are you looking for free and easy to use toolkits on Causal Pathway Diagrams, Prioritizing Implementation Barriers, Rapid Ethnographic Assessment, or Rapid Evidence Synthesis? Look no further than ImpSciMethods.org!
Implementation Science Methods for the Real World
Pragmatic, free, user-friendly implementation science toolkits to close the research to practice gap.
ImpSciMethods.org
June 17, 2025 at 6:26 PM
Hi #impsci friends! Are you looking for free and easy to use toolkits on Causal Pathway Diagrams, Prioritizing Implementation Barriers, Rapid Ethnographic Assessment, or Rapid Evidence Synthesis? Look no further than ImpSciMethods.org!
Reposted by Junqiang(John) Zhao
In the excitement over our new review of PAs, I forgot to tell you about the OTHER paper published in BMJ today, my commentary on the challenges of doing systematic reviews of evidence when there's no RCTs and most of the primary studies were unique and non-standardised.🧪
www.bmj.com/content/388/...
www.bmj.com/content/388/...

Systematic reviews of non-RCT evidence: building dry stone walls
To bake good cookies, start with good cookie dough. To use a different metaphor, to build a brick wall, take a large collection of bricks—all the same size and in perfect shape—and line them up neatly...
www.bmj.com
March 7, 2025 at 10:39 AM
In the excitement over our new review of PAs, I forgot to tell you about the OTHER paper published in BMJ today, my commentary on the challenges of doing systematic reviews of evidence when there's no RCTs and most of the primary studies were unique and non-standardised.🧪
www.bmj.com/content/388/...
www.bmj.com/content/388/...
Reposted by Junqiang(John) Zhao
Hot off the press for holiday reading! 🤓
We apply #criticalrealist #thematicanalysis to identify #mechanisms driving #implementation of a #CHW screening program. #Qualitative data can and should produce generalizable insights!
#impsci
implementationscience.biomedcentral.com/articles/10....
We apply #criticalrealist #thematicanalysis to identify #mechanisms driving #implementation of a #CHW screening program. #Qualitative data can and should produce generalizable insights!
#impsci
implementationscience.biomedcentral.com/articles/10....
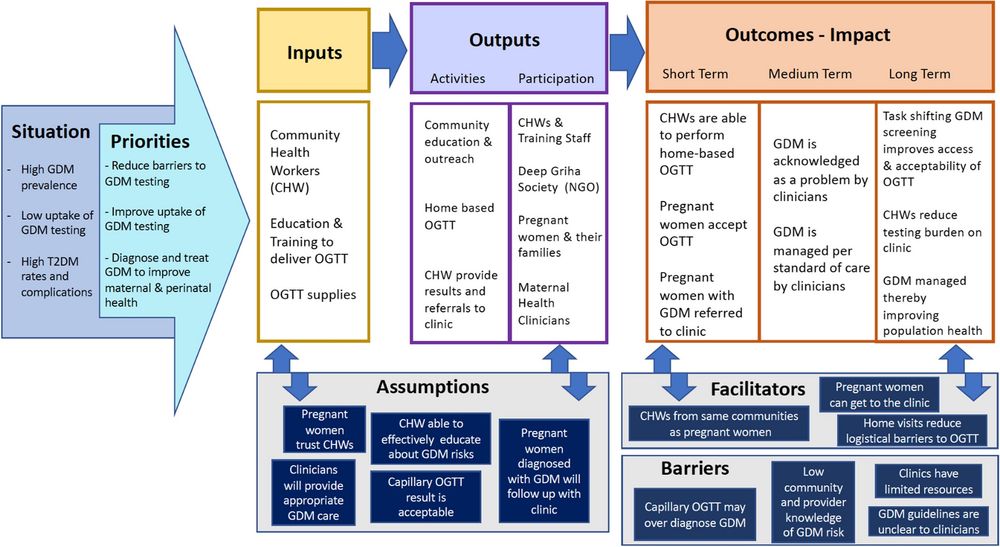
Generalizing from qualitative data: a case example using critical realist thematic analysis and mechanism mapping to evaluate a community health worker-led screening program in India - Implementation ...
Background A central goal of implementation science is to generate insights that allow evidence-based practices to be successfully applied across diverse settings. However, challenges often arise in p...
implementationscience.biomedcentral.com
December 24, 2024 at 9:42 PM
Hot off the press for holiday reading! 🤓
We apply #criticalrealist #thematicanalysis to identify #mechanisms driving #implementation of a #CHW screening program. #Qualitative data can and should produce generalizable insights!
#impsci
implementationscience.biomedcentral.com/articles/10....
We apply #criticalrealist #thematicanalysis to identify #mechanisms driving #implementation of a #CHW screening program. #Qualitative data can and should produce generalizable insights!
#impsci
implementationscience.biomedcentral.com/articles/10....
#impsci folks. Worth reading and reflection on this default barrier/ enabler analysis approach in our doing of implementation research
Loving this paper 'Rethinking barriers and enablers'. How many thousands of weak research studies have reduced complex change to 'identifying and addressing barriers and enablers'? Here's how to do better!
journals.sagepub.com/doi/full/10....
journals.sagepub.com/doi/full/10....

Rethinking Barriers and Enablers in Qualitative Health Research: Limitations, Alternatives, and Enhancements - Abby Haynes, Victoria Loblay, 2024
Explorations of barriers and enablers (or barriers and facilitators) to a desired health practice, implementation process, or intervention outcome have become s...
journals.sagepub.com
November 20, 2024 at 11:53 AM
#impsci folks. Worth reading and reflection on this default barrier/ enabler analysis approach in our doing of implementation research


