
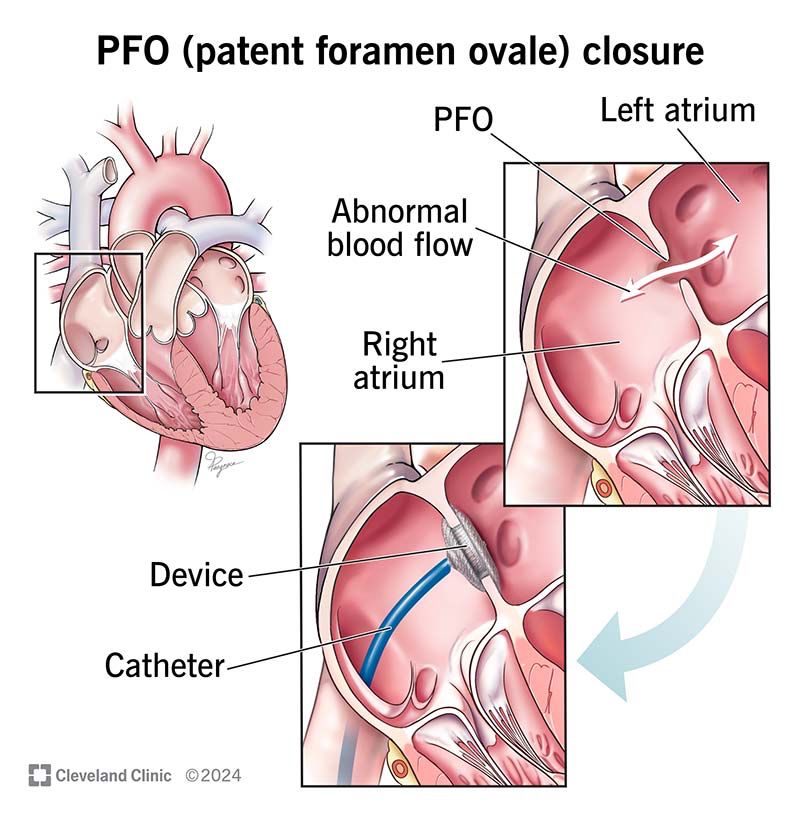
Not necessarily. About 20% of the population has a PFO. Most strokes, even in patients with a PFO, were probably from something else.
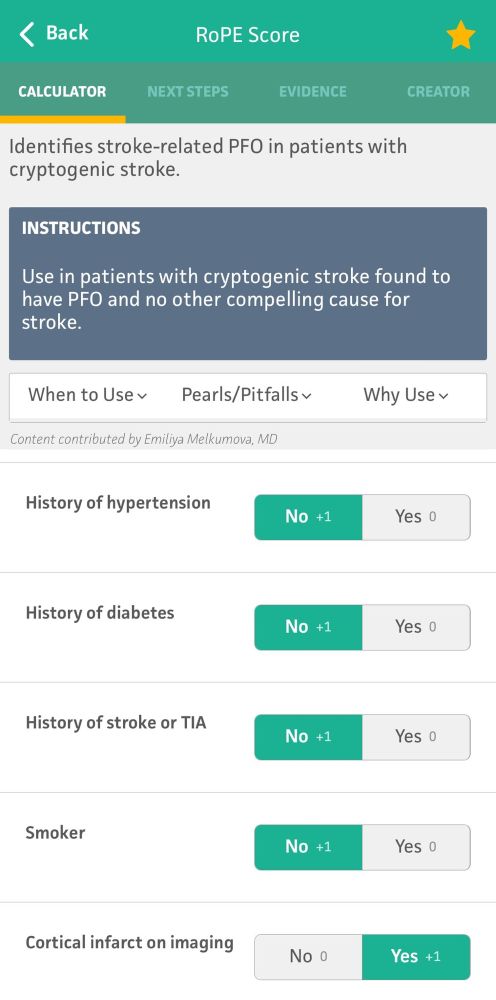
The decision to close one is based off of size, imaging, patient age and risk, and scoring tools (eg RoPE score).
Not necessarily. About 20% of the population has a PFO. Most strokes, even in patients with a PFO, were probably from something else.
The decision to close one is based off of size, imaging, patient age and risk, and scoring tools (eg RoPE score).
Most afib patients require chronic anticoagulation, and this is doubly true for stroke patients. Studies have shown superiority in DOACs (eg apixaban) over warfarin. If patients have contraindications to chronic AC, a LAA occlusive device gets almost the same benefit.
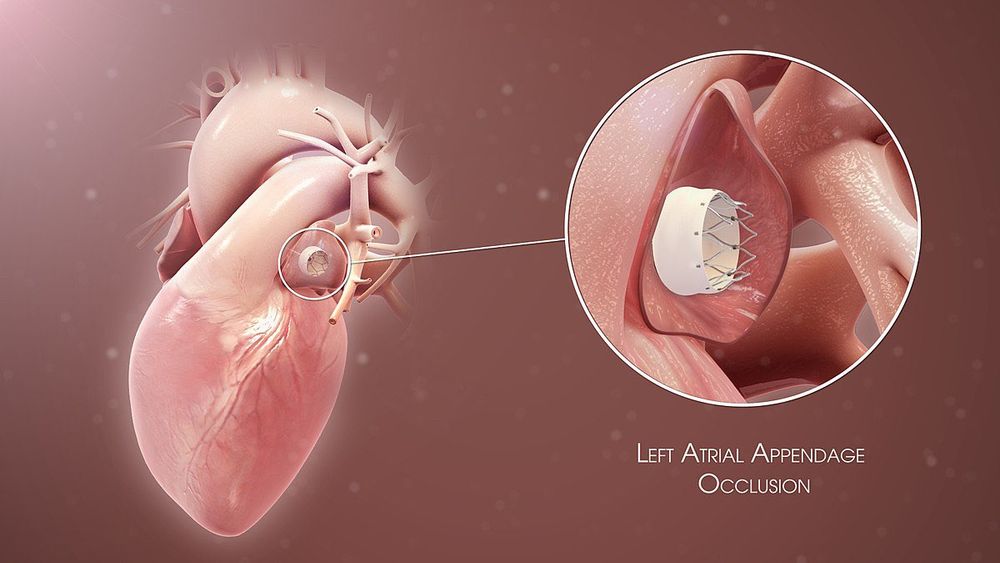
Most afib patients require chronic anticoagulation, and this is doubly true for stroke patients. Studies have shown superiority in DOACs (eg apixaban) over warfarin. If patients have contraindications to chronic AC, a LAA occlusive device gets almost the same benefit.

The thrombi from cardioembolic strokes are typically larger than atheroembolic strokes (see pt 1) meaning the strokes generally fall in large vessel territories (not lacunes).
The unique feature is that it can hit any vascular territory, left/right/anterior posterior.
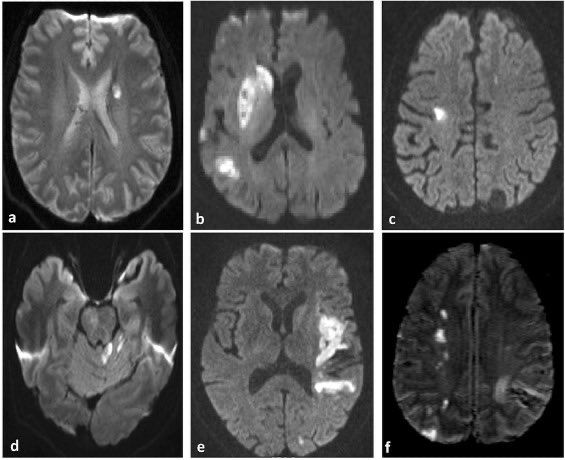
The thrombi from cardioembolic strokes are typically larger than atheroembolic strokes (see pt 1) meaning the strokes generally fall in large vessel territories (not lacunes).
The unique feature is that it can hit any vascular territory, left/right/anterior posterior.
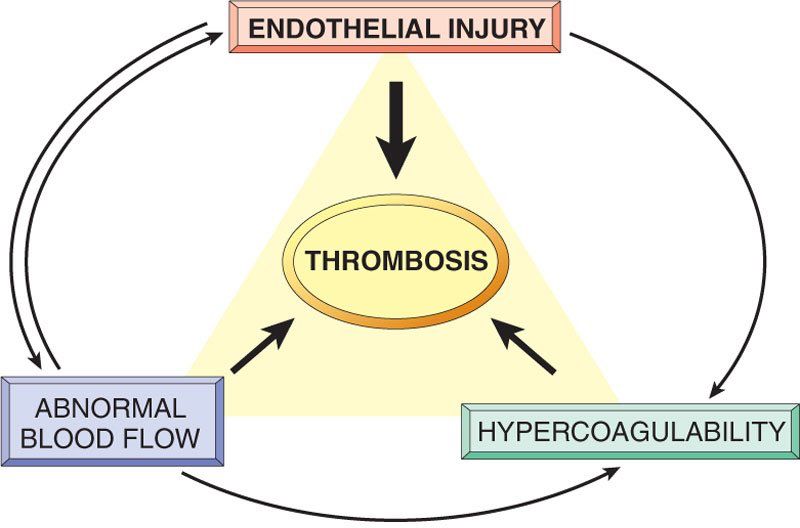
Cardioembolic strokes are generally caused by the other two corners of Virchow’s triad: stasis (eg afib) and hypercoagulability (eg paradoxical embolus from a DVT). Overactivity of secondary coagulation results in a thrombus which can embolize.
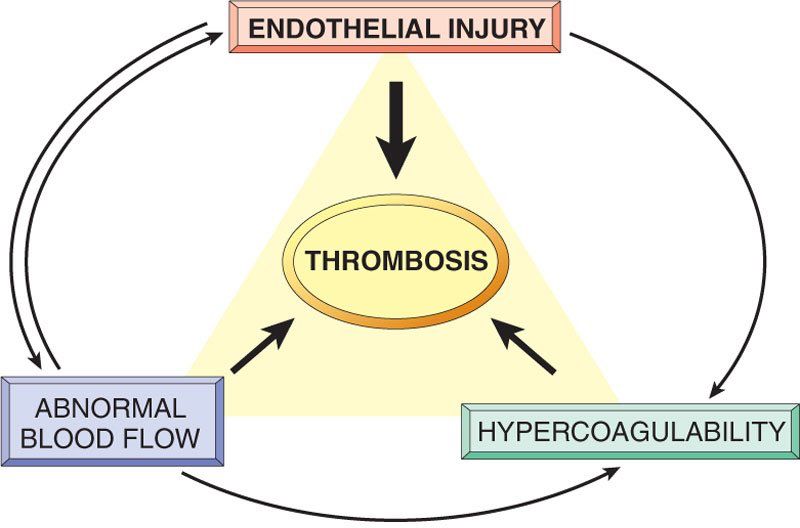
Cardioembolic strokes are generally caused by the other two corners of Virchow’s triad: stasis (eg afib) and hypercoagulability (eg paradoxical embolus from a DVT). Overactivity of secondary coagulation results in a thrombus which can embolize.
These patients are also treated with lifelong single antiplatelet therapy (remember Virchow’s triad).
DAPT has a slight benefit but only in the very short term (ie 21 days).
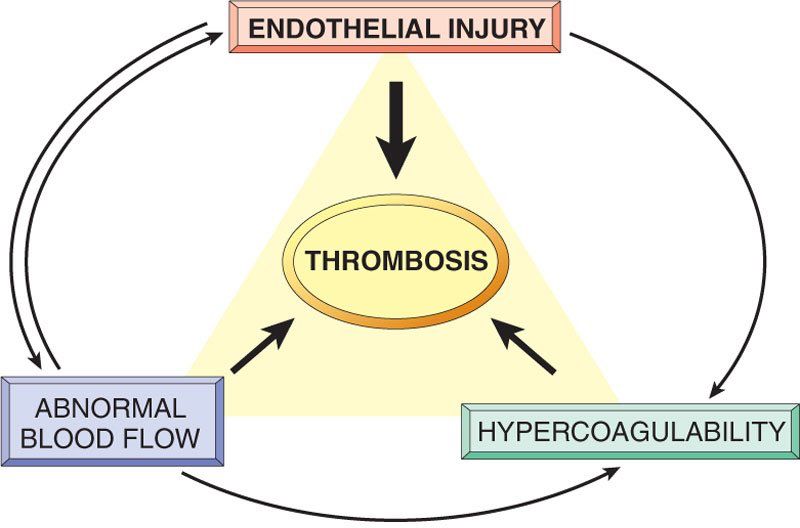
These patients are also treated with lifelong single antiplatelet therapy (remember Virchow’s triad).
DAPT has a slight benefit but only in the very short term (ie 21 days).
1. “Holes” of dead tissue (lacunes)
2. Enlarged perivascular spaces
3. White matter hyperintensities (on T2 weighted imaging)
These findings may be too subtle to pick up on CT, though.
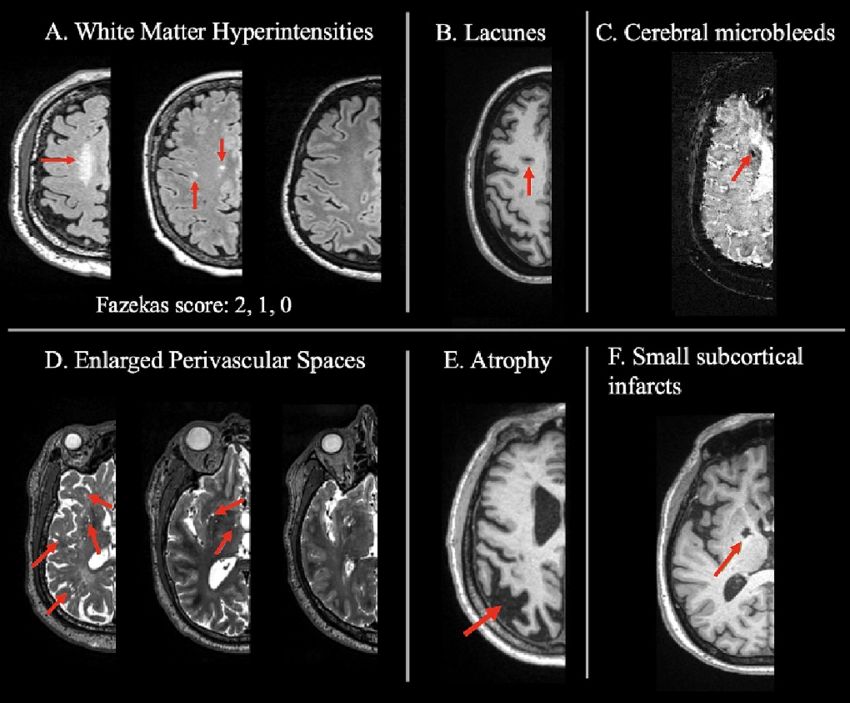
1. “Holes” of dead tissue (lacunes)
2. Enlarged perivascular spaces
3. White matter hyperintensities (on T2 weighted imaging)
These findings may be too subtle to pick up on CT, though.


1. Lipohyalinosis -> arteriosclerosis and occlusion
2. Branch atheroma with distal occlusion
The second is probable easier to understand: atheromatous disease can block off these branches at the proximal supply.

1. Lipohyalinosis -> arteriosclerosis and occlusion
2. Branch atheroma with distal occlusion
The second is probable easier to understand: atheromatous disease can block off these branches at the proximal supply.
Small vessel occlusions refer to ischemic strokes impacting vessels too small to have names. These small perforating arteries are at right angles to larger vessels and primarily supply the basal ganglia, thalami, white matter, and brainstem.

Small vessel occlusions refer to ischemic strokes impacting vessels too small to have names. These small perforating arteries are at right angles to larger vessels and primarily supply the basal ganglia, thalami, white matter, and brainstem.

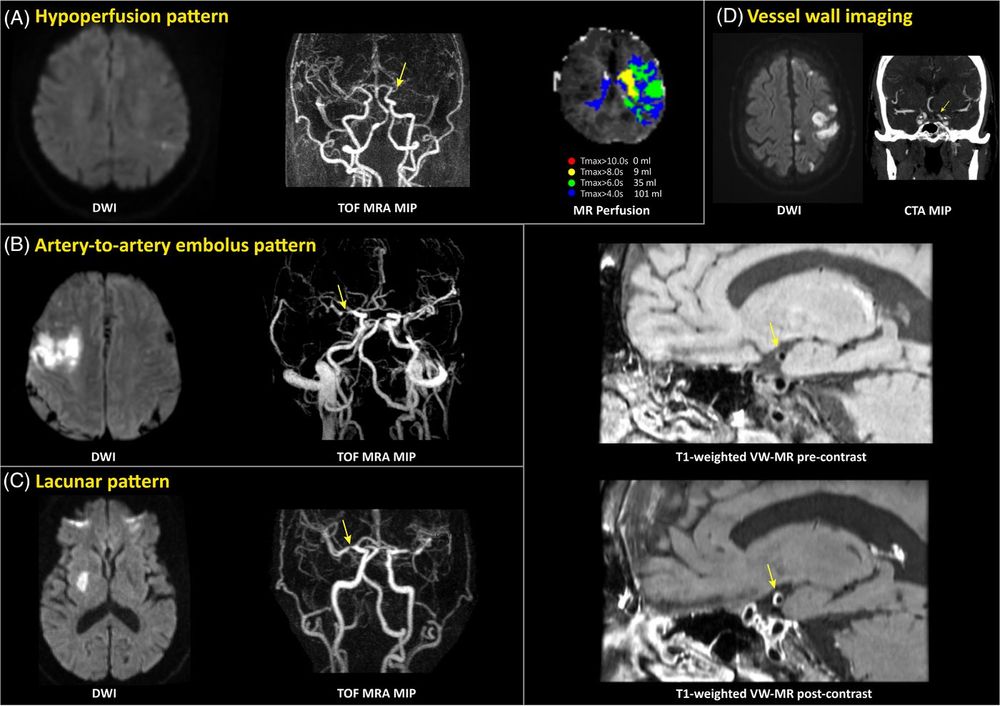
LAA is diagnosed based on imaging characteristics, both of the stroke itself and the blood vessels. The latter is critical for management, meaning we need vessel imaging to work it up.
Options include:
- CTA (preferred)
- MRA
- Carotid ultrasound

LAA is diagnosed based on imaging characteristics, both of the stroke itself and the blood vessels. The latter is critical for management, meaning we need vessel imaging to work it up.
Options include:
- CTA (preferred)
- MRA
- Carotid ultrasound
LAA is caused by the same common pathway that often causes other vascular diseases including MIs and PVD: atherosclerosis.
Risk factors include anything that causes vessel trauma: HTN, diabetes, smoking, FHx, and high LDL. It accounts for about 25% of strokes in the USA.

LAA is caused by the same common pathway that often causes other vascular diseases including MIs and PVD: atherosclerosis.
Risk factors include anything that causes vessel trauma: HTN, diabetes, smoking, FHx, and high LDL. It accounts for about 25% of strokes in the USA.
Let’s start with large artery atherosclerosis.

Let’s start with large artery atherosclerosis.
The cerebellum receives inputs from 3 sources: eyes, inner ear, and nerves. If any one system goes down, you have a backup. If 2 go down, or if the cerebellum goes out, you have a problem.

The cerebellum receives inputs from 3 sources: eyes, inner ear, and nerves. If any one system goes down, you have a backup. If 2 go down, or if the cerebellum goes out, you have a problem.
There are also variants designed to increase sensitivity in special situations.

There are also variants designed to increase sensitivity in special situations.



- Bazett
- Hodges
- Fridericia
- Framingham
- Rautaharju

- Bazett
- Hodges
- Fridericia
- Framingham
- Rautaharju
Medulla: ASA (M) + PICA (S)
Pons: basilar (M) + AICA (S)
Midbrain: SCA (inf M/S) + PCA (sup M/S)

Medulla: ASA (M) + PICA (S)
Pons: basilar (M) + AICA (S)
Midbrain: SCA (inf M/S) + PCA (sup M/S)
- Anteromedial (paramedian)
- Anterolateral (short circumferential)
- Lateral (long circumferential)
- Posterior

- Anteromedial (paramedian)
- Anterolateral (short circumferential)
- Lateral (long circumferential)
- Posterior

