Heather Gustafson
@heatherhg.bsky.social
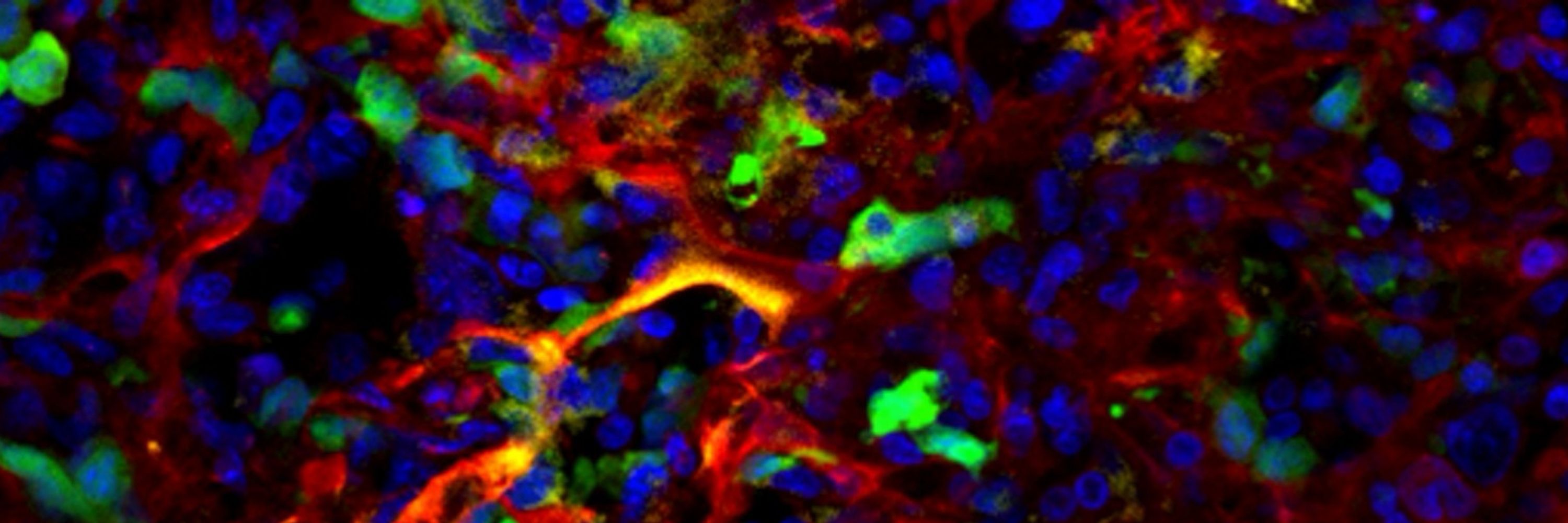
Scientist. Engineer. Mom. Wife. Lover of macrophages. #EoE and rare eosinophilic disease daughter, patient, and mom. Finding a love of eosinophils. Trying to help kids with cancer, running a lab at #UW and #SeattleChildrens: Editlabs.org . Views are my own
7/
Key takeaway: all patients had inflammation post-CAR, but outcomes were shaped by their immune system’s ability to manage it.
We need new strategies to support immune recovery and limit harmful inflammation during CAR T therapy.
More is not always better.
End of thread.
Key takeaway: all patients had inflammation post-CAR, but outcomes were shaped by their immune system’s ability to manage it.
We need new strategies to support immune recovery and limit harmful inflammation during CAR T therapy.
More is not always better.
End of thread.
May 20, 2025 at 7:32 PM
7/
Key takeaway: all patients had inflammation post-CAR, but outcomes were shaped by their immune system’s ability to manage it.
We need new strategies to support immune recovery and limit harmful inflammation during CAR T therapy.
More is not always better.
End of thread.
Key takeaway: all patients had inflammation post-CAR, but outcomes were shaped by their immune system’s ability to manage it.
We need new strategies to support immune recovery and limit harmful inflammation during CAR T therapy.
More is not always better.
End of thread.
6/
Our model:
Patients with sufficient cell numbers dampen inflammation and do well
Those with just enough cells respond, but develop toxicity
Patients with too few cells fail to respond and have runaway inflammation
Our model:
Patients with sufficient cell numbers dampen inflammation and do well
Those with just enough cells respond, but develop toxicity
Patients with too few cells fail to respond and have runaway inflammation
May 20, 2025 at 7:32 PM
6/
Our model:
Patients with sufficient cell numbers dampen inflammation and do well
Those with just enough cells respond, but develop toxicity
Patients with too few cells fail to respond and have runaway inflammation
Our model:
Patients with sufficient cell numbers dampen inflammation and do well
Those with just enough cells respond, but develop toxicity
Patients with too few cells fail to respond and have runaway inflammation
5/
We also noticed more severe cytopenias in the dysfunctional and toxic groups.
It appears that when patients have fewer immune cells, they can't buffer or "adsorb" the cytokines generated by therapy.
We also noticed more severe cytopenias in the dysfunctional and toxic groups.
It appears that when patients have fewer immune cells, they can't buffer or "adsorb" the cytokines generated by therapy.

May 20, 2025 at 7:32 PM
5/
We also noticed more severe cytopenias in the dysfunctional and toxic groups.
It appears that when patients have fewer immune cells, they can't buffer or "adsorb" the cytokines generated by therapy.
We also noticed more severe cytopenias in the dysfunctional and toxic groups.
It appears that when patients have fewer immune cells, they can't buffer or "adsorb" the cytokines generated by therapy.
4/
Yes. Higher cytokine levels correlated with worse survival, even after adjusting for tumor burden.
Inflammation wasn’t just a consequence of disease—it was part of the prognosis.
Yes. Higher cytokine levels correlated with worse survival, even after adjusting for tumor burden.
Inflammation wasn’t just a consequence of disease—it was part of the prognosis.

May 20, 2025 at 7:32 PM
4/
Yes. Higher cytokine levels correlated with worse survival, even after adjusting for tumor burden.
Inflammation wasn’t just a consequence of disease—it was part of the prognosis.
Yes. Higher cytokine levels correlated with worse survival, even after adjusting for tumor burden.
Inflammation wasn’t just a consequence of disease—it was part of the prognosis.
3/
Patients with toxicity "caught up" to the dysfunctional group by day 7—suggesting that the therapy itself is driving inflammation.
But we also saw high levels of inflammation in patients who responded to CAR T without severe toxicity. Could inflammation be a general predictor of poor outcomes?
Patients with toxicity "caught up" to the dysfunctional group by day 7—suggesting that the therapy itself is driving inflammation.
But we also saw high levels of inflammation in patients who responded to CAR T without severe toxicity. Could inflammation be a general predictor of poor outcomes?
May 20, 2025 at 7:32 PM
3/
Patients with toxicity "caught up" to the dysfunctional group by day 7—suggesting that the therapy itself is driving inflammation.
But we also saw high levels of inflammation in patients who responded to CAR T without severe toxicity. Could inflammation be a general predictor of poor outcomes?
Patients with toxicity "caught up" to the dysfunctional group by day 7—suggesting that the therapy itself is driving inflammation.
But we also saw high levels of inflammation in patients who responded to CAR T without severe toxicity. Could inflammation be a general predictor of poor outcomes?
2/
So we analyzed cytokine and immune response data from days 1, 3, and 7 after CAR T-cell infusion.
What we found was surprising: all patients were inflamed, regardless of clinical outcome.
In fact, the most inflammation was in dysfunctional patients.
So we analyzed cytokine and immune response data from days 1, 3, and 7 after CAR T-cell infusion.
What we found was surprising: all patients were inflamed, regardless of clinical outcome.
In fact, the most inflammation was in dysfunctional patients.

May 20, 2025 at 7:32 PM
2/
So we analyzed cytokine and immune response data from days 1, 3, and 7 after CAR T-cell infusion.
What we found was surprising: all patients were inflamed, regardless of clinical outcome.
In fact, the most inflammation was in dysfunctional patients.
So we analyzed cytokine and immune response data from days 1, 3, and 7 after CAR T-cell infusion.
What we found was surprising: all patients were inflamed, regardless of clinical outcome.
In fact, the most inflammation was in dysfunctional patients.
1/
We hypothesized that patients fall along a spectrum of inflammatory responses:
High inflammation = functional CAR response with toxicity
Balanced inflammation = functional CAR response without toxicity
Low or ineffective inflammation = dysfunctional or no CAR response
We hypothesized that patients fall along a spectrum of inflammatory responses:
High inflammation = functional CAR response with toxicity
Balanced inflammation = functional CAR response without toxicity
Low or ineffective inflammation = dysfunctional or no CAR response
May 20, 2025 at 7:32 PM
1/
We hypothesized that patients fall along a spectrum of inflammatory responses:
High inflammation = functional CAR response with toxicity
Balanced inflammation = functional CAR response without toxicity
Low or ineffective inflammation = dysfunctional or no CAR response
We hypothesized that patients fall along a spectrum of inflammatory responses:
High inflammation = functional CAR response with toxicity
Balanced inflammation = functional CAR response without toxicity
Low or ineffective inflammation = dysfunctional or no CAR response

