Interested in physiology, medical education, LGBTQ+ health, and the kidneys.
Skeets are my own/not medical advice. 🏳️🌈



🧠 Score 20-30 = poor prognosis (short-course recommended)
🧠 Score 30-35 = intermediate prognosis
🧠 Score 36-45 = favorable prognosis (longer course recommended, as more likely to recur)
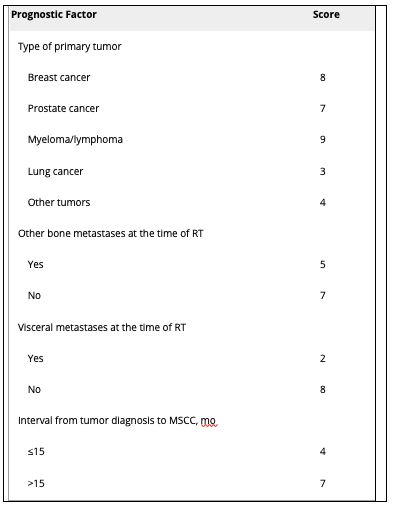
🧠 Score 20-30 = poor prognosis (short-course recommended)
🧠 Score 30-35 = intermediate prognosis
🧠 Score 36-45 = favorable prognosis (longer course recommended, as more likely to recur)
🧠 MRI w/in 24 hrs: sagittal T1 and T2-weighted sequence of whole spine + axial imaging of detected lesions
🧠 CT + myelogram if MRI contraindicated
🧠 Bladder scan if relevant + Foley if needed
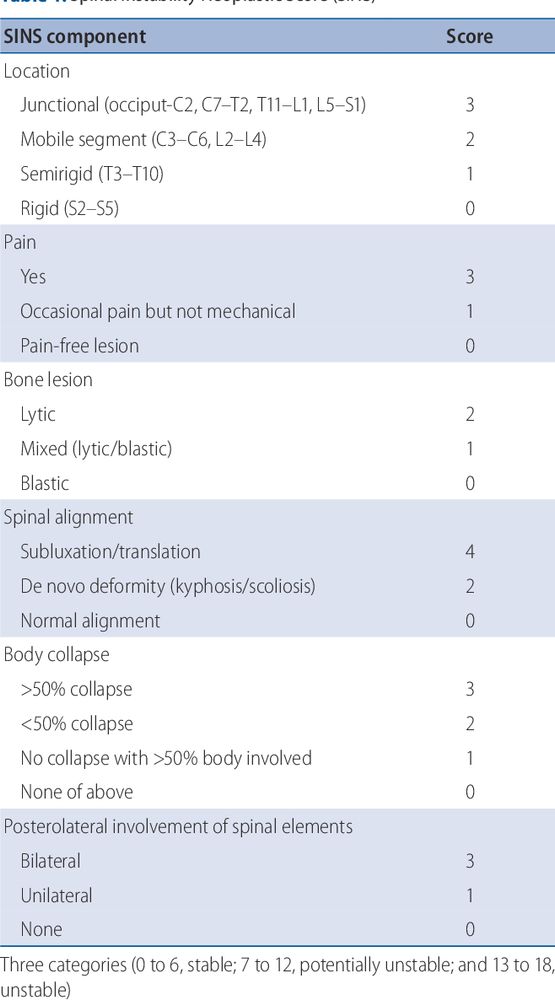
🧠 Assess for spinal instability (e.g. Spinal Instability Neoplastic Score)
🧠 MRI w/in 24 hrs: sagittal T1 and T2-weighted sequence of whole spine + axial imaging of detected lesions
🧠 CT + myelogram if MRI contraindicated
🧠 Bladder scan if relevant + Foley if needed
🧠 Assess for spinal instability (e.g. Spinal Instability Neoplastic Score)
Back pain is the most common symptom.
🧠 Severe and localized
🧠 Worse when coughing, sneezing, defecating or lying down
🧠 Progressive worsening
🧠 Disturbs sleep
Other features
🧠 Weakness
🧠 Sensory disturbance
🧠 Autonomic dysfunction
🧠 Paralysis
🧠 Cauda equina syndrome
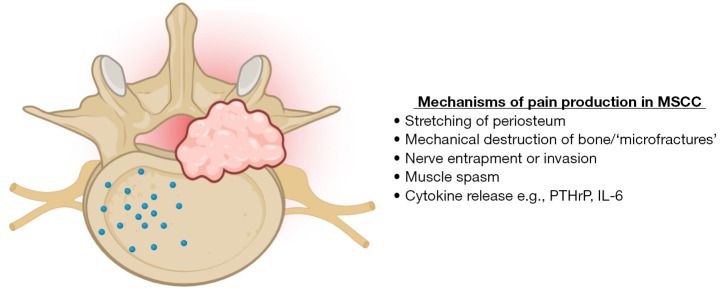
Back pain is the most common symptom.
🧠 Severe and localized
🧠 Worse when coughing, sneezing, defecating or lying down
🧠 Progressive worsening
🧠 Disturbs sleep
Other features
🧠 Weakness
🧠 Sensory disturbance
🧠 Autonomic dysfunction
🧠 Paralysis
🧠 Cauda equina syndrome
🫀 The Kishi scoring system
- Score >3 indicates need for stenting
🫀 The Yu grading system
- Score of 3 or 4 indicates need for stenting
🫀The Stanford Method
- Venography used to identify patients at risk for airway or brain involvement
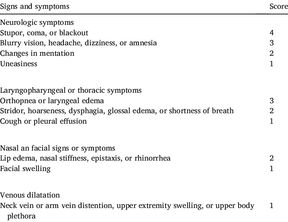

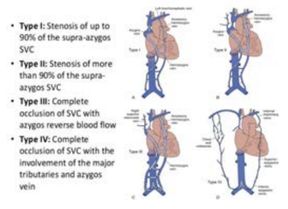
🫀 The Kishi scoring system
- Score >3 indicates need for stenting
🫀 The Yu grading system
- Score of 3 or 4 indicates need for stenting
🫀The Stanford Method
- Venography used to identify patients at risk for airway or brain involvement
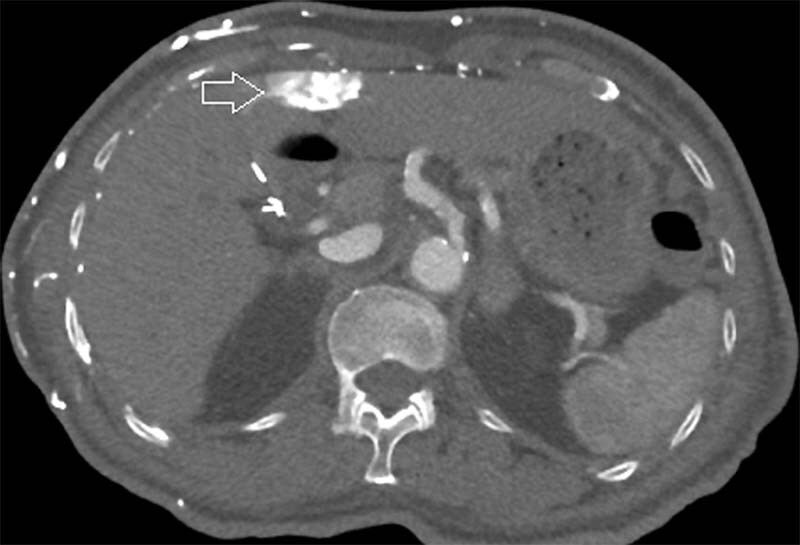
🫀SVC drains blood from the brachiocephalic veins, which receive blood from the head and upper extremities
🫀Collateral supply is important in SVC syndrome
🫀Upper/mid esophageal veins drain into the esophagus, causing "downhill esophageal varices"
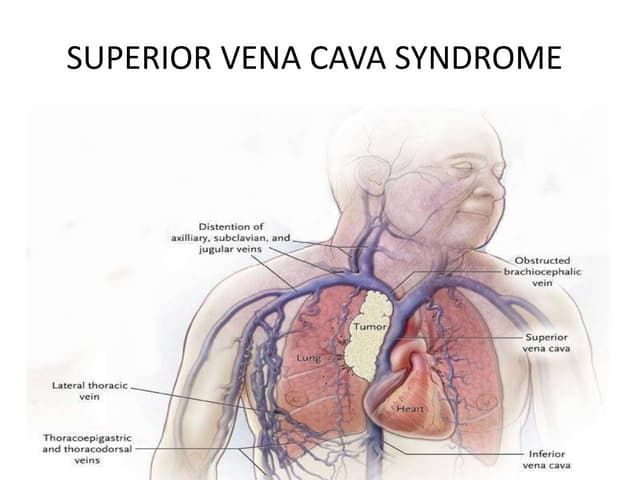
🫀SVC drains blood from the brachiocephalic veins, which receive blood from the head and upper extremities
🫀Collateral supply is important in SVC syndrome
🫀Upper/mid esophageal veins drain into the esophagus, causing "downhill esophageal varices"
🩸Leukostasis = symptomatic hyperleukocytosis (WBC >100,000)
🩸Clinical features = respiratory and neurological symptoms
🩸May cause falsely high K, low O2, and high platelets
🩸Definitive treatment = induction chemo but perform bone marrow bx first
🩸Use hydroxurea while awaiting studies

🩸Leukostasis = symptomatic hyperleukocytosis (WBC >100,000)
🩸Clinical features = respiratory and neurological symptoms
🩸May cause falsely high K, low O2, and high platelets
🩸Definitive treatment = induction chemo but perform bone marrow bx first
🩸Use hydroxurea while awaiting studies
🩸Respiratory distress
🩸Neurological changes
🩸Other end organ damage
🩸Hyperleukocytosis
Novotny et. al (2005) created the attached grading score to predict the probability of leukostasis.
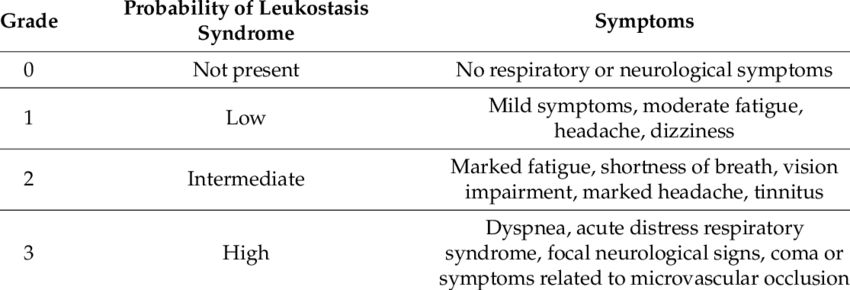
🩸Respiratory distress
🩸Neurological changes
🩸Other end organ damage
🩸Hyperleukocytosis
Novotny et. al (2005) created the attached grading score to predict the probability of leukostasis.
🌡️ Known source: usual duration + ANC is improving and >500
🌡️ Unknown source: no fever for >2 days + ANC is improving and >500
Prophylaxis:
🌡️ IDSA guidelines regarding prophylaxis are outlined in the attached table.

🌡️ Known source: usual duration + ANC is improving and >500
🌡️ Unknown source: no fever for >2 days + ANC is improving and >500
Prophylaxis:
🌡️ IDSA guidelines regarding prophylaxis are outlined in the attached table.
🌡️ Meropenem/imipenem
🌡️ Vancomycin
🌡️ Aminoglycoside or ciprofloxacin
Only use vancomycin if:
🌡️ Skin/soft tissue infection
🌡️ Catheter-related infection
🌡️ Pneumonia
🌡️ Hemodynamically unstable
Add antifungal if no response within 3-7 days.

🌡️ Meropenem/imipenem
🌡️ Vancomycin
🌡️ Aminoglycoside or ciprofloxacin
Only use vancomycin if:
🌡️ Skin/soft tissue infection
🌡️ Catheter-related infection
🌡️ Pneumonia
🌡️ Hemodynamically unstable
Add antifungal if no response within 3-7 days.
🌡️ Once blood cultures are drawn, start empiric antibiotics within 1 hr
Inpatient:
🌡️ Empiric cefepime, pip-tazo, or meropenem is recommended
🌡️ Severe penicillin allergy: ciprofloxacin + clindamycin
🌡️ Broaden if suspected MDRO
Outpatient:
🌡️ Ciprofloxacin + Augmentin

🌡️ Once blood cultures are drawn, start empiric antibiotics within 1 hr
Inpatient:
🌡️ Empiric cefepime, pip-tazo, or meropenem is recommended
🌡️ Severe penicillin allergy: ciprofloxacin + clindamycin
🌡️ Broaden if suspected MDRO
Outpatient:
🌡️ Ciprofloxacin + Augmentin
1. MASCC Scoring System
📋 Score <21 = inpatient
2. Talcott's rules
📋 Groups I-III = inpatient
📋Group IV low-risk = outpatient
3. CISNE
📋 Used for stable pts receiving mild-mod chemo for solid malignancy
📋 Score >2 = inpatient




1. MASCC Scoring System
📋 Score <21 = inpatient
2. Talcott's rules
📋 Groups I-III = inpatient
📋Group IV low-risk = outpatient
3. CISNE
📋 Used for stable pts receiving mild-mod chemo for solid malignancy
📋 Score >2 = inpatient
🦀 Stones (nephrolithiasis)
🦀 Groans (abdominal pain, N/V, pancreatitis)
🦀 Bones (bone pain, muscle weakness)
🦀 Psychiatric overtones (depression, anxiety)
🦀 Cardiac manifestations (short QT, bradycardia, AVN blockade)
🦀 Nephrogenic DI (polyuria, thirst)


🦀 Stones (nephrolithiasis)
🦀 Groans (abdominal pain, N/V, pancreatitis)
🦀 Bones (bone pain, muscle weakness)
🦀 Psychiatric overtones (depression, anxiety)
🦀 Cardiac manifestations (short QT, bradycardia, AVN blockade)
🦀 Nephrogenic DI (polyuria, thirst)
Options:
🦀 Rasburicase
🦀 Allopurinol
🦀 Febuxostat
🦀 Dialysis
🦀 Rasburicase is preferred over allopurinol
- Faster acting
- Allopurinol does not remove existing uric acid and leads to buildup of xanthine (also nephrotoxic)
🦀 But, rasburicase is contraindicated in G6PD deficiency

Options:
🦀 Rasburicase
🦀 Allopurinol
🦀 Febuxostat
🦀 Dialysis
🦀 Rasburicase is preferred over allopurinol
- Faster acting
- Allopurinol does not remove existing uric acid and leads to buildup of xanthine (also nephrotoxic)
🦀 But, rasburicase is contraindicated in G6PD deficiency
🦀 BMP (Cr, BUN, K, Phos, and Ca)
🦀 CBC (WBC, may also have anemia/thrombocytopenia)
🦀 Uric Acid
🦀 EKG
🦀 LDH
🦀 Urinalysis + urine microscopy
TLS is diagnosed via the Cairo-Bishop Classification:
🦀 Laboratory (asymptomatic)
🦀 Clinical (symptomatic)

🦀 BMP (Cr, BUN, K, Phos, and Ca)
🦀 CBC (WBC, may also have anemia/thrombocytopenia)
🦀 Uric Acid
🦀 EKG
🦀 LDH
🦀 Urinalysis + urine microscopy
TLS is diagnosed via the Cairo-Bishop Classification:
🦀 Laboratory (asymptomatic)
🦀 Clinical (symptomatic)
🫀Cardiac myocytes have glucagon receptors
🫀These receptors also act through Gs proteins to activate PKA, providing the above benefits even in the setting of BB or CCB toxicity

🫀Cardiac myocytes have glucagon receptors
🫀These receptors also act through Gs proteins to activate PKA, providing the above benefits even in the setting of BB or CCB toxicity
🫀L-type Ca channels open ➡️ Ca binds RyR ➡️ Ca released from sarcoplasmic reticulum
🫀Ca binds troponin C ➡️ exposes myosin-binding site of actin
🫀SERCA2 pumps Ca back into SR
🫀Phospholamban inhibits SERCA2


🫀L-type Ca channels open ➡️ Ca binds RyR ➡️ Ca released from sarcoplasmic reticulum
🫀Ca binds troponin C ➡️ exposes myosin-binding site of actin
🫀SERCA2 pumps Ca back into SR
🫀Phospholamban inhibits SERCA2
📝Elderly patients
📝Pts with underlying kidney disease
📝Volume depletion (dehydration, diuretic use)
📝Use of ACEi or ARBs
📝Use of K-sparing diuretics (spironolactone)

📝Elderly patients
📝Pts with underlying kidney disease
📝Volume depletion (dehydration, diuretic use)
📝Use of ACEi or ARBs
📝Use of K-sparing diuretics (spironolactone)
📝 In patients with CKD, renal clearance of AVN blockers is impaired
📝 Underlying CKD + AVN blockade (+ARB in this case) ➡️ HyperK
📝 HyperK + AVN blockade ➡️ bradycardia + shock

📝 In patients with CKD, renal clearance of AVN blockers is impaired
📝 Underlying CKD + AVN blockade (+ARB in this case) ➡️ HyperK
📝 HyperK + AVN blockade ➡️ bradycardia + shock
T3
🫀⬇️FFA beta-oxidation
🫀⬇️CYP7A1, leading to impaired cholesterol clearance
🫀⬇️Lipoprotein Lipase, decreasing hydrolysis of VLDL
TSH
🫀⬇️CYP7A1
🫀⬆️PCSK9
🫀⬆️HMG CoA reductase
🫀⬆️Hormone-Sensitive lipase


T3
🫀⬇️FFA beta-oxidation
🫀⬇️CYP7A1, leading to impaired cholesterol clearance
🫀⬇️Lipoprotein Lipase, decreasing hydrolysis of VLDL
TSH
🫀⬇️CYP7A1
🫀⬆️PCSK9
🫀⬆️HMG CoA reductase
🫀⬆️Hormone-Sensitive lipase
🫀Slow conduction speeds
🫀Delayed and prolonged repolarization phase
🫀Hypothermia may also block the transient outward current responsible for Phase 1 of the cardiac AP


🫀Slow conduction speeds
🫀Delayed and prolonged repolarization phase
🫀Hypothermia may also block the transient outward current responsible for Phase 1 of the cardiac AP
🫀Bradycardia
🫀Long PQ segment
🫀Diffuse flattened or inverted T waves
🫀Low voltage QRS
🫀AV blockage
🫀Acquired long QT syndrome, which can lead to TdP
🫀Osborn waves

🫀Bradycardia
🫀Long PQ segment
🫀Diffuse flattened or inverted T waves
🫀Low voltage QRS
🫀AV blockage
🫀Acquired long QT syndrome, which can lead to TdP
🫀Osborn waves
What are the physiologic mechanisms underlying these associations?
Welcome to another #PhysiologyFriday!
A 🧵
#MedSky #CardioSky

What are the physiologic mechanisms underlying these associations?
Welcome to another #PhysiologyFriday!
A 🧵
#MedSky #CardioSky


