Chetan Shenoy
@cshenoy.bsky.social
Cardiologist and researcher, in cardiovascular magnetic resonance imaging, at the University of Minnesota
Pinned
Chetan Shenoy
@cshenoy.bsky.social
· May 24
academic.oup.com/eurheartj/ad...
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
Reposted by Chetan Shenoy
Important multicenter study in #EHJ
#CMR outperforms societal recs for ICD placement in cardiac sarcoidosis
📈AUC=0.86 for 5-yr risk of fatal/life-threatening arrhythmias
⚡Highest risk = abnl LVEF + LGE that is multifocal, septal, subepicardial, or involves RV freewall
buff.ly/Nc2upbU
#cardiotwitter
#CMR outperforms societal recs for ICD placement in cardiac sarcoidosis
📈AUC=0.86 for 5-yr risk of fatal/life-threatening arrhythmias
⚡Highest risk = abnl LVEF + LGE that is multifocal, septal, subepicardial, or involves RV freewall
buff.ly/Nc2upbU
#cardiotwitter

September 30, 2025 at 11:02 PM
Important multicenter study in #EHJ
#CMR outperforms societal recs for ICD placement in cardiac sarcoidosis
📈AUC=0.86 for 5-yr risk of fatal/life-threatening arrhythmias
⚡Highest risk = abnl LVEF + LGE that is multifocal, septal, subepicardial, or involves RV freewall
buff.ly/Nc2upbU
#cardiotwitter
#CMR outperforms societal recs for ICD placement in cardiac sarcoidosis
📈AUC=0.86 for 5-yr risk of fatal/life-threatening arrhythmias
⚡Highest risk = abnl LVEF + LGE that is multifocal, septal, subepicardial, or involves RV freewall
buff.ly/Nc2upbU
#cardiotwitter
Reposted by Chetan Shenoy
Must-watch lecture on cardiomyopathy and CMR by @cshenoy.bsky.social
„more often than what is the EF we should ask the why?“
youtube.com/live/9or85hk...
„more often than what is the EF we should ask the why?“
youtube.com/live/9or85hk...
Identifying the Cause of Cardiomyopathy Using CMR (Chetan Shenoy, MBBS, MS)
YouTube video by Houston Methodist DeBakey CV Education
youtube.com
July 19, 2025 at 5:40 AM
Must-watch lecture on cardiomyopathy and CMR by @cshenoy.bsky.social
„more often than what is the EF we should ask the why?“
youtube.com/live/9or85hk...
„more often than what is the EF we should ask the why?“
youtube.com/live/9or85hk...
Reposted by Chetan Shenoy
“CMR phenotyping can be used immediately in clinical practice to identify patients with suspected cardiac sarcoidosis who would benefit from a primary prevention ICD," said Chetan Shenoy, MD. Read more about how this can prevent life-threatening ventricular arrhythmias: www.tctmd.com/news/cmr-may...
CMR May Improve Assessment of ICD Need in Cardiac Sarcoidosis
The imaging was better than societal recommendations at discriminating long-term risk of ventricular arrhythmias.
www.tctmd.com
June 19, 2025 at 1:09 PM
“CMR phenotyping can be used immediately in clinical practice to identify patients with suspected cardiac sarcoidosis who would benefit from a primary prevention ICD," said Chetan Shenoy, MD. Read more about how this can prevent life-threatening ventricular arrhythmias: www.tctmd.com/news/cmr-may...
Thank you, @toddneale.bsky.social, for your excellent reporting on our EHJ paper!
@tctmd.bsky.social @escardio.bsky.social @paragbawaskar.bsky.social
@tctmd.bsky.social @escardio.bsky.social @paragbawaskar.bsky.social
CMR May Improve Assessment of ICD Need in Cardiac Sarcoidosis

CMR May Improve Assessment of ICD Need in Cardiac Sarcoidosis
CMR May Improve Assessment of ICD Need in Cardiac Sarcoidosis
cmacahilig@crf.org
Wed, 06/11/2025 - 16:08
Todd Neale
The imaging was better than societal recommendations at discriminating long-term risk of ventricular arrhythmias.
www.tctmd.com
June 11, 2025 at 10:12 PM
Thank you, @toddneale.bsky.social, for your excellent reporting on our EHJ paper!
@tctmd.bsky.social @escardio.bsky.social @paragbawaskar.bsky.social
@tctmd.bsky.social @escardio.bsky.social @paragbawaskar.bsky.social
Reposted by Chetan Shenoy
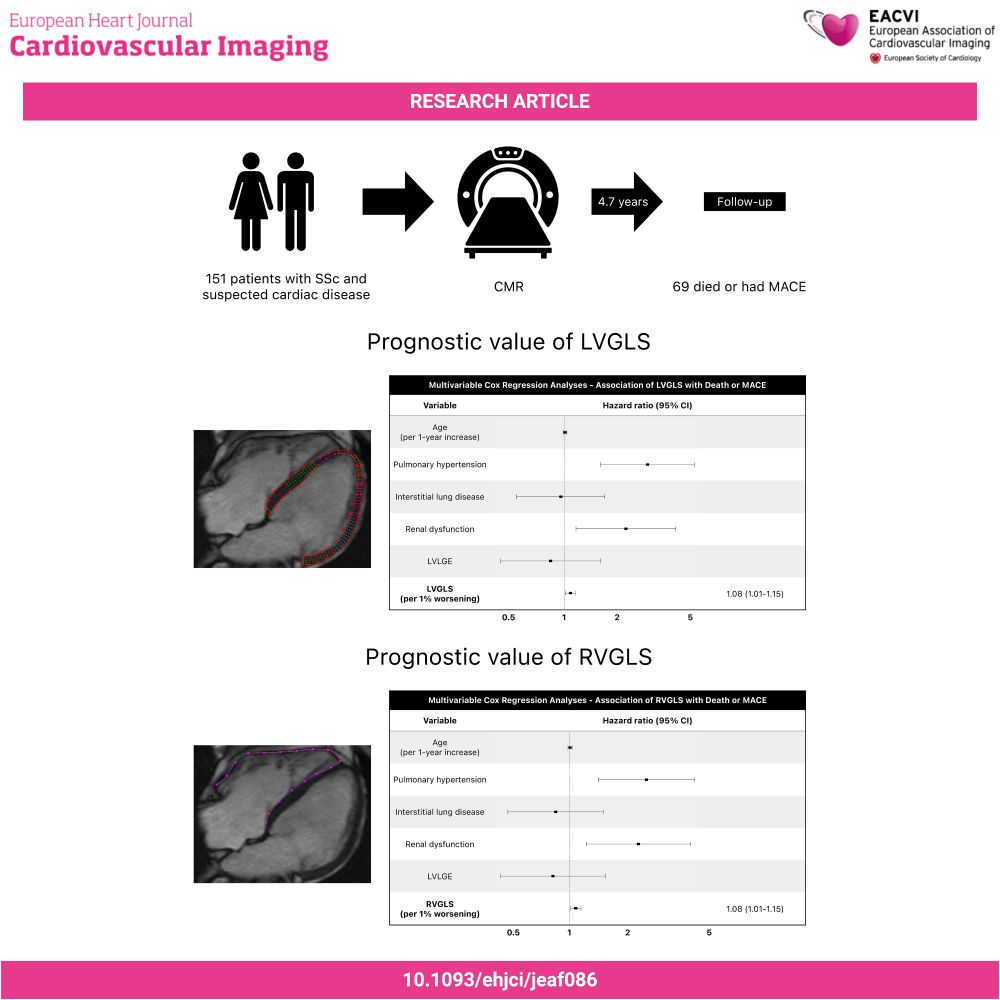
#EHJCVI 🫀 What's the value of ventricular strain in systemic sclerosis? 📉 Both LVGLS and RVGLS are linked to death or MACE, unlike LVEF and RVEF 🧠 How does strain compare to traditional prognostic markers? 🔍 Read more 👉 doi.org/10.1093/ehjc... #CardioSky @jgrapsa.bsky.social @escardio.bsky.social
June 10, 2025 at 9:02 PM
#EHJCVI 🫀 What's the value of ventricular strain in systemic sclerosis? 📉 Both LVGLS and RVGLS are linked to death or MACE, unlike LVEF and RVEF 🧠 How does strain compare to traditional prognostic markers? 🔍 Read more 👉 doi.org/10.1093/ehjc... #CardioSky @jgrapsa.bsky.social @escardio.bsky.social
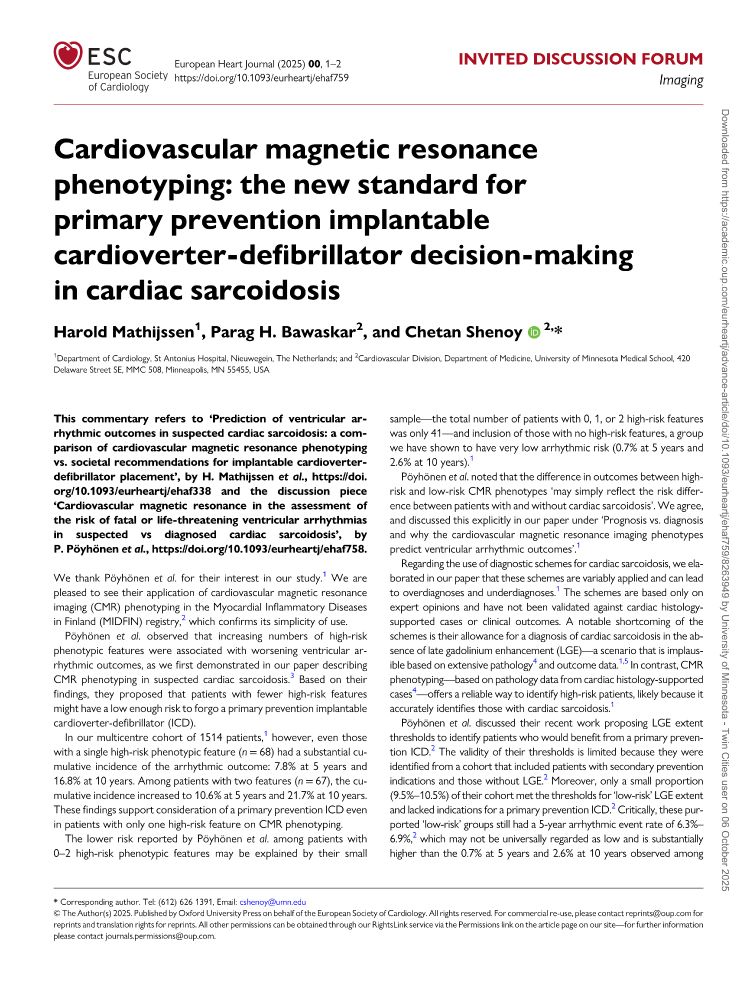
Prediction of ventricular arrhythmic outcomes in suspected cardiac sarcoidosis: a comparison of cardiovascular magnetic resonance phenotyping vs. societal recommendations for implantable cardioverter-defibrillator placement
academic.oup.com/eurheartj/ad...
#Cardiosky #WhyCMR #Epeeps #Medsky
academic.oup.com/eurheartj/ad...
#Cardiosky #WhyCMR #Epeeps #Medsky

May 27, 2025 at 1:32 PM
Prediction of ventricular arrhythmic outcomes in suspected cardiac sarcoidosis: a comparison of cardiovascular magnetic resonance phenotyping vs. societal recommendations for implantable cardioverter-defibrillator placement
academic.oup.com/eurheartj/ad...
#Cardiosky #WhyCMR #Epeeps #Medsky
academic.oup.com/eurheartj/ad...
#Cardiosky #WhyCMR #Epeeps #Medsky
Reposted by Chetan Shenoy
Cardiac sarcoidosis is a undervalued disease and difficult to diagnose and treat, considering potential life-threatening arrhythmias. Nice to have some more guidance.
#cardiosky.
#cardiosky.
academic.oup.com/eurheartj/ad...
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
May 25, 2025 at 7:09 AM
Cardiac sarcoidosis is a undervalued disease and difficult to diagnose and treat, considering potential life-threatening arrhythmias. Nice to have some more guidance.
#cardiosky.
#cardiosky.
academic.oup.com/eurheartj/ad...
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
May 24, 2025 at 2:39 PM
academic.oup.com/eurheartj/ad...
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
@escardio.bsky.social
#Cardiosky #WhyCMR #Epeeps #Medsky
Please DM me if you would like a full-text PDF of the paper!
Reposted by Chetan Shenoy
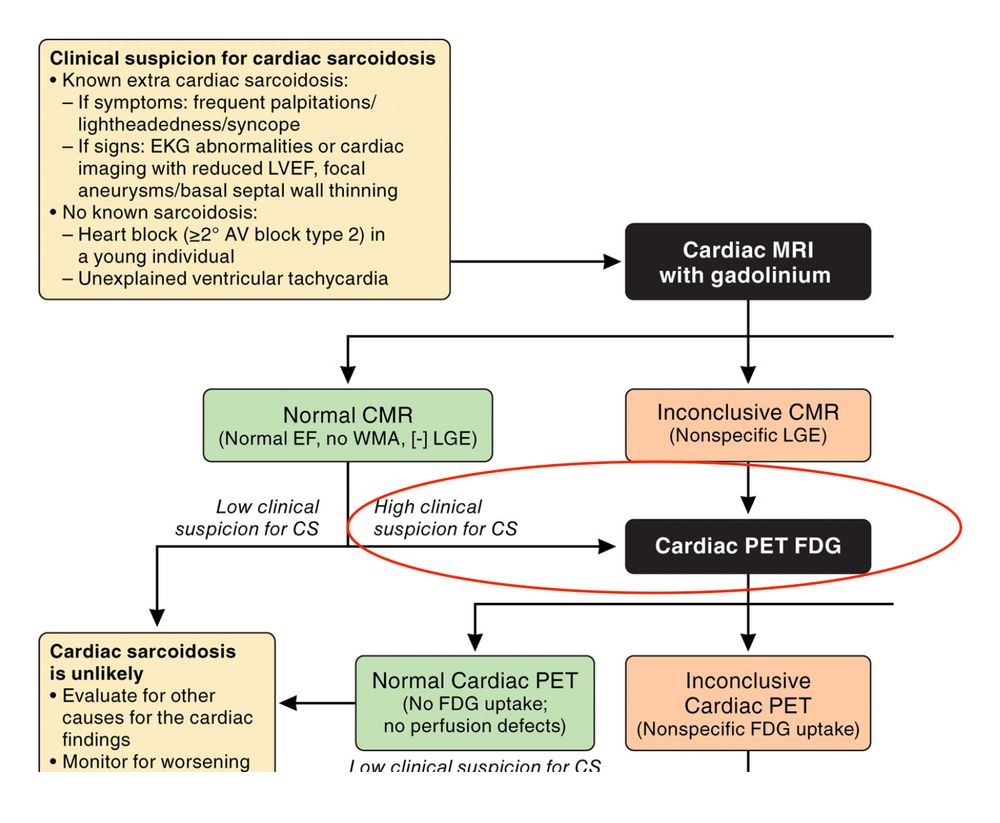
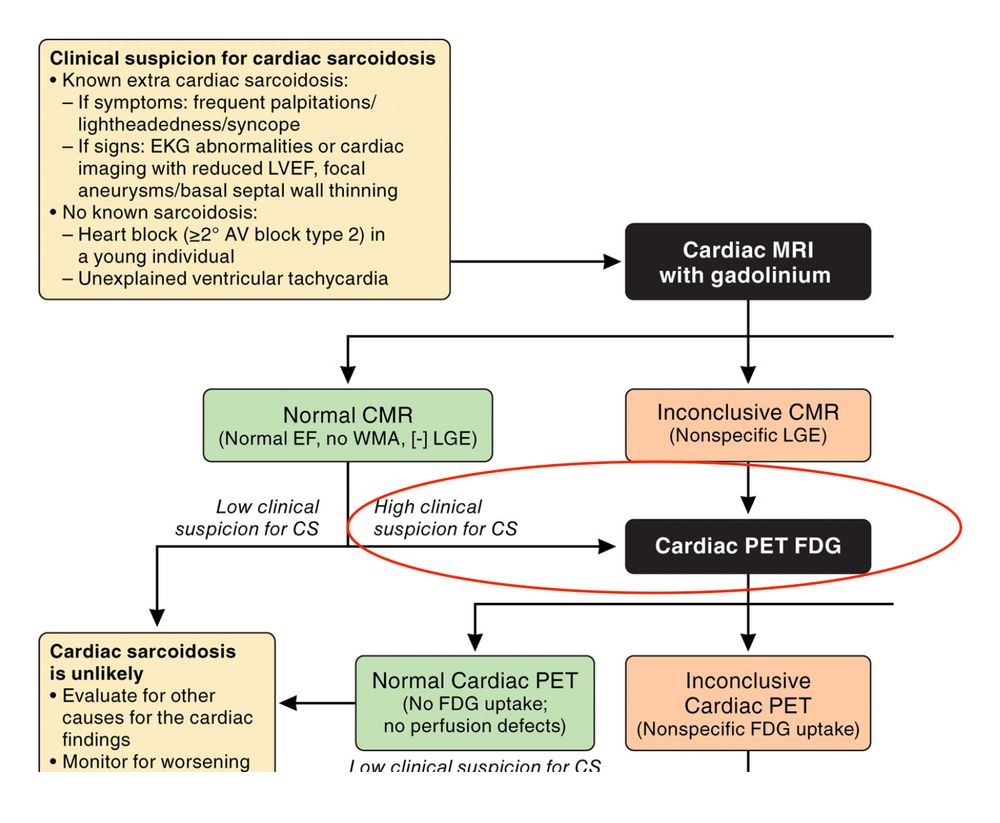
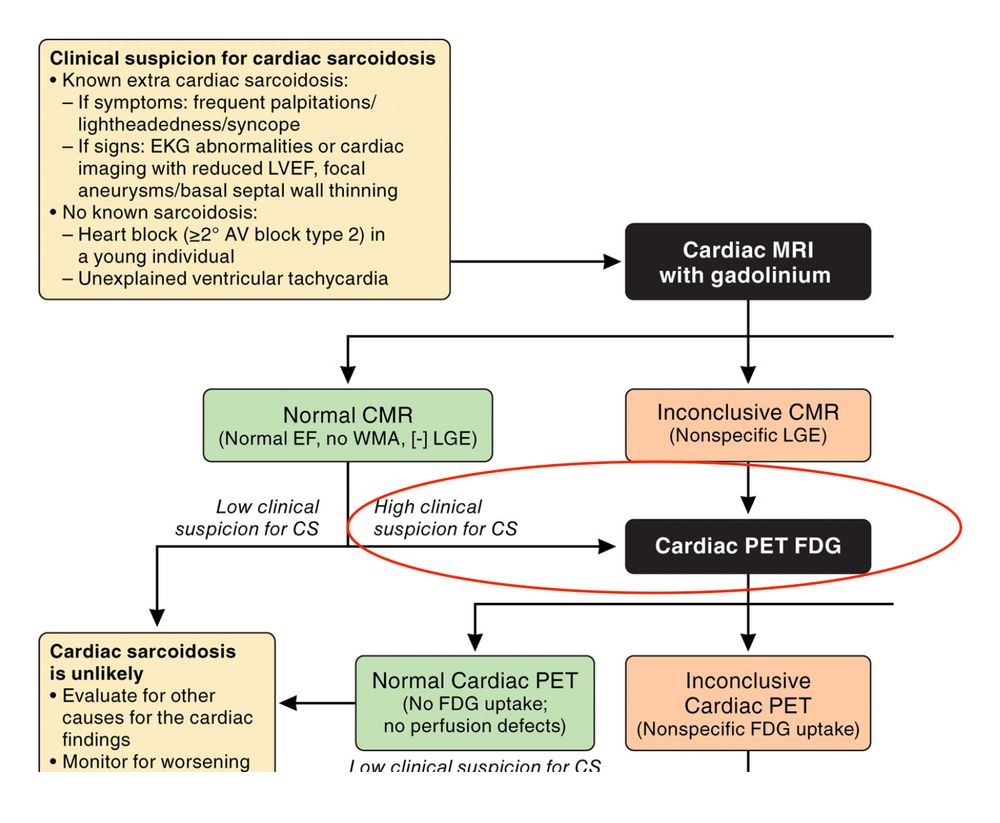
In patients with suspected cardiac sarcoidosis, cardiac FDG-PET is recommended after a normal CMR if there is a high clinical suspicion. What are the data supporting this recommendation? #CardioSky #MedSky #Sarcoidosis
March 21, 2025 at 11:39 PM
In patients with suspected cardiac sarcoidosis, cardiac FDG-PET is recommended after a normal CMR if there is a high clinical suspicion. What are the data supporting this recommendation? #CardioSky #MedSky #Sarcoidosis
Reposted by Chetan Shenoy
Query sarcoid, normal #WhyCMR, so then should we do FDG-PET? Not much benefit.
In patients with suspected cardiac sarcoidosis, cardiac FDG-PET is recommended after a normal CMR if there is a high clinical suspicion. What are the data supporting this recommendation? #CardioSky #MedSky #Sarcoidosis
March 23, 2025 at 5:29 AM
Query sarcoid, normal #WhyCMR, so then should we do FDG-PET? Not much benefit.
In patients with suspected cardiac sarcoidosis, cardiac FDG-PET is recommended after a normal CMR if there is a high clinical suspicion. What are the data supporting this recommendation? #CardioSky #MedSky #Sarcoidosis
March 21, 2025 at 11:39 PM
In patients with suspected cardiac sarcoidosis, cardiac FDG-PET is recommended after a normal CMR if there is a high clinical suspicion. What are the data supporting this recommendation? #CardioSky #MedSky #Sarcoidosis
This paper reports the coexistence of cardiac sarcoidosis and arrhythmogenic cardiomyopathy in 5 patients.
heart.bmj.com/content/earl...
#CardioSky #MedSky
heart.bmj.com/content/earl...
#CardioSky #MedSky

Coexistence of cardiac sarcoidosis and arrhythmogenic cardiomyopathy-associated genetic variants: a multicentre case-control study
Background Cardiac sarcoidosis (CS) is a chronic inflammatory disease characterised by non-caseating granulomas, while arrhythmogenic cardiomyopathy (ACM) is a genetic condition mainly affecting desmo...
heart.bmj.com
January 23, 2025 at 2:08 AM
This paper reports the coexistence of cardiac sarcoidosis and arrhythmogenic cardiomyopathy in 5 patients.
heart.bmj.com/content/earl...
#CardioSky #MedSky
heart.bmj.com/content/earl...
#CardioSky #MedSky
Reposted by Chetan Shenoy
Great thread on LV thrombus and embolism risk - especially if RWMA I discuss lifelong anti coagulation with my pts even if it looks resolved on echo, good to have some data to help back this up 👇
In 2019, we wrote a paper showing that patients with left ventricular thrombus have a long-term risk of embolism, extending to at least 8 years.
We were puzzled by the finding…
#CardioSky
www.ahajournals.org/doi/10.1161/...
We were puzzled by the finding…
#CardioSky
www.ahajournals.org/doi/10.1161/...

November 21, 2024 at 7:49 AM
Great thread on LV thrombus and embolism risk - especially if RWMA I discuss lifelong anti coagulation with my pts even if it looks resolved on echo, good to have some data to help back this up 👇
Amazing achievement by rising star and post-doc in my lab @paragbawaskar.bsky.social, winner of the prestigious 2024 Melvin Judkins Early Career Investigator Award at #AHA24!! Congratulations!!!
@ahascience.bsky.social
@ahascience.bsky.social


November 17, 2024 at 3:46 PM
Amazing achievement by rising star and post-doc in my lab @paragbawaskar.bsky.social, winner of the prestigious 2024 Melvin Judkins Early Career Investigator Award at #AHA24!! Congratulations!!!
@ahascience.bsky.social
@ahascience.bsky.social
Reposted by Chetan Shenoy
It’s great that journals are coming over here, but what I have really missed after my departure from Twitter 2 years ago is this, the authors themselves presenting their works and discussing it with peers. #cardiosky #medsky #emimcc
In 2019, we wrote a paper showing that patients with left ventricular thrombus have a long-term risk of embolism, extending to at least 8 years.
We were puzzled by the finding…
#CardioSky
www.ahajournals.org/doi/10.1161/...
We were puzzled by the finding…
#CardioSky
www.ahajournals.org/doi/10.1161/...

November 13, 2024 at 3:58 PM
It’s great that journals are coming over here, but what I have really missed after my departure from Twitter 2 years ago is this, the authors themselves presenting their works and discussing it with peers. #cardiosky #medsky #emimcc
Reposted by Chetan Shenoy
With the big caveat that obvious alternative causes are not present such as AF.
November 13, 2024 at 9:03 PM
With the big caveat that obvious alternative causes are not present such as AF.
Reposted by Chetan Shenoy
All patients with stroke is unrealistic in terms of cost, access and resourcing.
However in patients with ischaemic stroke, LV dysfunction and/or recent MI I agree (if #echofirst + contrast is negative for thrombus).
However in patients with ischaemic stroke, LV dysfunction and/or recent MI I agree (if #echofirst + contrast is negative for thrombus).
November 13, 2024 at 9:02 PM
All patients with stroke is unrealistic in terms of cost, access and resourcing.
However in patients with ischaemic stroke, LV dysfunction and/or recent MI I agree (if #echofirst + contrast is negative for thrombus).
However in patients with ischaemic stroke, LV dysfunction and/or recent MI I agree (if #echofirst + contrast is negative for thrombus).
Reposted by Chetan Shenoy
Thanks for your insights. Fascinating area.
November 13, 2024 at 6:42 AM
Thanks for your insights. Fascinating area.
Reposted by Chetan Shenoy
Thanks. So for example - post anterior infarct, persisting WMA on CMR at 6 months despite OMT (but improvement in overall LVEF). Lifelong anticoagulation or would you reimage at a further interval (I.e. 12 months) to look for improvement in wall motion abnormality?
November 13, 2024 at 6:31 AM
Thanks. So for example - post anterior infarct, persisting WMA on CMR at 6 months despite OMT (but improvement in overall LVEF). Lifelong anticoagulation or would you reimage at a further interval (I.e. 12 months) to look for improvement in wall motion abnormality?
Reposted by Chetan Shenoy
Great work Chetan. An important area where as a community we need to get better at managing - particularly in the post (anterior) STEMI space. What are your thoughts on stopping anticoagulation at 3 or 6 months post MI with persisting wall motion defects but resolved thrombus?
November 13, 2024 at 6:17 AM
Great work Chetan. An important area where as a community we need to get better at managing - particularly in the post (anterior) STEMI space. What are your thoughts on stopping anticoagulation at 3 or 6 months post MI with persisting wall motion defects but resolved thrombus?
Reposted by Chetan Shenoy
Congratulations for this work! Do you have data for patients with CMR and echo to evaluate the discrepancy?
We need a well designed RCT to answer this important although infrequent question. And to assess the effectiveness of DOAC in these cases
We need a well designed RCT to answer this important although infrequent question. And to assess the effectiveness of DOAC in these cases
November 13, 2024 at 6:54 AM
Congratulations for this work! Do you have data for patients with CMR and echo to evaluate the discrepancy?
We need a well designed RCT to answer this important although infrequent question. And to assess the effectiveness of DOAC in these cases
We need a well designed RCT to answer this important although infrequent question. And to assess the effectiveness of DOAC in these cases