Amy Gleichman
@amygleichman.bsky.social
Neuroscientist / astrocyte enthusiast / fan of new viral tools 🧠
Assistant Professor, Ohio State
GleichmanLab.com
Assistant Professor, Ohio State
GleichmanLab.com
You’re not sorry 😂 and thanks! Hope to catch up one of these days
October 11, 2025 at 4:42 AM
You’re not sorry 😂 and thanks! Hope to catch up one of these days
Thanks, Wendy!!
October 10, 2025 at 11:22 PM
Thanks, Wendy!!
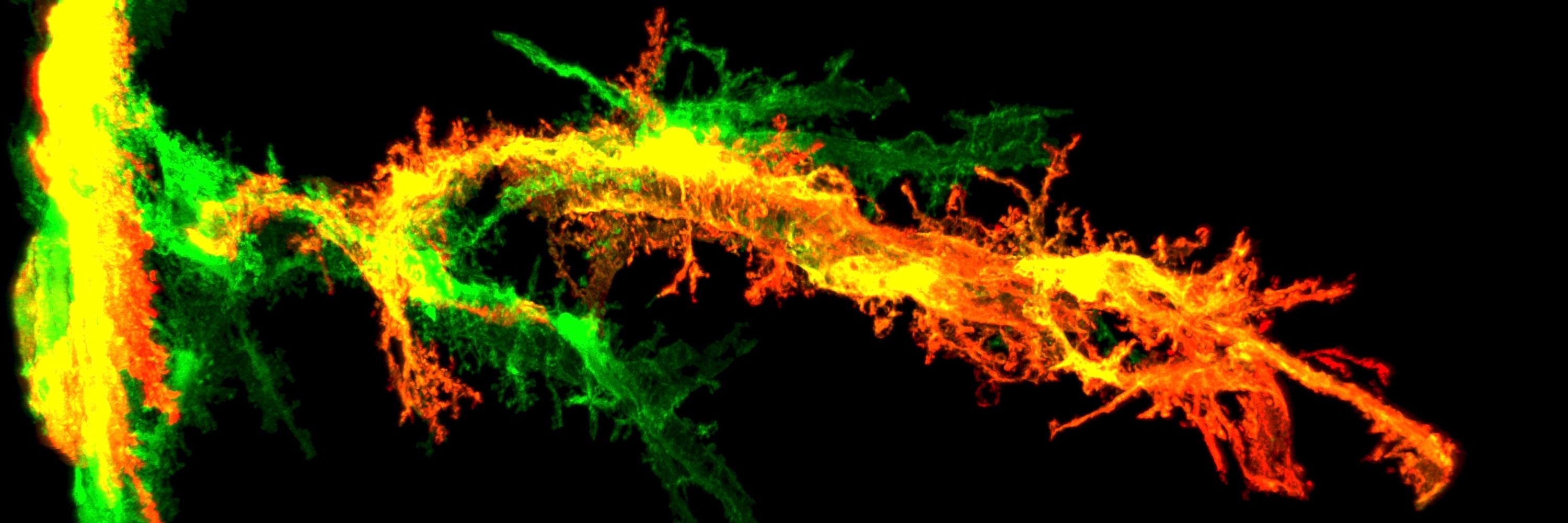
And finally, a couple of virally-labeled astrocytes, because they are just so pretty. Red is a cortical astrocyte, green is a white matter astrocyte.

October 10, 2025 at 11:13 PM
And finally, a couple of virally-labeled astrocytes, because they are just so pretty. Red is a cortical astrocyte, green is a white matter astrocyte.
I started my own lab about 6 months ago at Ohio State where we’re continuing to look at ways to manipulate astrocyte biology to improve brain repair. We’re also generating new viral tools along the way, for use in research and hopefully in gene therapies for patients down the line.
October 10, 2025 at 11:13 PM
I started my own lab about 6 months ago at Ohio State where we’re continuing to look at ways to manipulate astrocyte biology to improve brain repair. We’re also generating new viral tools along the way, for use in research and hopefully in gene therapies for patients down the line.
Take-home message: astrocytes can respond in nuanced ways even to very similar injuries, and those nuances can be leveraged for interventions. Huge thank you to my postdoc mentor, Tom Carmichael, as well as our amazing collaborators Michael Sofroniew, Riki Kawaguchi, and Elle Rathbun.
October 10, 2025 at 11:13 PM
Take-home message: astrocytes can respond in nuanced ways even to very similar injuries, and those nuances can be leveraged for interventions. Huge thank you to my postdoc mentor, Tom Carmichael, as well as our amazing collaborators Michael Sofroniew, Riki Kawaguchi, and Elle Rathbun.
Looks like yes! Overexpression of Lamc1 in white matter astrocytes led to a smaller fibrotic scar and axotomized region as well as behavioral improvements. This also changed the immune cells entering the area, with a huge increase in Tregs. Overall, Lamc1 in white matter astrocytes improved repair.
October 10, 2025 at 11:13 PM
Looks like yes! Overexpression of Lamc1 in white matter astrocytes led to a smaller fibrotic scar and axotomized region as well as behavioral improvements. This also changed the immune cells entering the area, with a huge increase in Tregs. Overall, Lamc1 in white matter astrocytes improved repair.
We made a lentivirus to overexpress Lamc1 in astrocytes and injected it in the white matter, and saw an increase in vascular remodeling specifically of those larger-caliber vessels. These are kind of weird vessels to have in white matter, which is more capillary-heavy. Are they a good thing?
October 10, 2025 at 11:13 PM
We made a lentivirus to overexpress Lamc1 in astrocytes and injected it in the white matter, and saw an increase in vascular remodeling specifically of those larger-caliber vessels. These are kind of weird vessels to have in white matter, which is more capillary-heavy. Are they a good thing?
So it looks like Lamc1 is an endogenous mechanism by which cortical astrocytes improve repair after stroke, and it’s acting specifically to increase remodeling of arterioles and venules. Can we leverage this to improve repair in white matter stroke, where this mechanism doesn’t usually turn on?
October 10, 2025 at 11:13 PM
So it looks like Lamc1 is an endogenous mechanism by which cortical astrocytes improve repair after stroke, and it’s acting specifically to increase remodeling of arterioles and venules. Can we leverage this to improve repair in white matter stroke, where this mechanism doesn’t usually turn on?
Surprisingly, we saw a pretty specific decrease in remodeling of arterioles and venules, but the capillary bed was unchanged. These vessels were all intact; knocking out Lamc1 didn’t affect blood-brain barrier permeability.
October 10, 2025 at 11:13 PM
Surprisingly, we saw a pretty specific decrease in remodeling of arterioles and venules, but the capillary bed was unchanged. These vessels were all intact; knocking out Lamc1 didn’t affect blood-brain barrier permeability.
Using a variety of metrics, we identified a pro-angiogenic gene (Lamc1) upregulated in cortical astrocytes near the stroke but not white matter astrocytes. We developed a dual-virus CRISPR system to knock it out in astrocytes in the cortex, and found a decrease in vascular remodeling post-stroke.
October 10, 2025 at 11:13 PM
Using a variety of metrics, we identified a pro-angiogenic gene (Lamc1) upregulated in cortical astrocytes near the stroke but not white matter astrocytes. We developed a dual-virus CRISPR system to knock it out in astrocytes in the cortex, and found a decrease in vascular remodeling post-stroke.
Vascular remodeling and angiogenesis after a cortical stroke improve brain repair. We’ve known astrocytes in the cortex can help this process (see great work from @m-r-williamson.bsky.social and Theresa Jones), but it’s less clear what’s going on in white matter.
October 10, 2025 at 11:13 PM
Vascular remodeling and angiogenesis after a cortical stroke improve brain repair. We’ve known astrocytes in the cortex can help this process (see great work from @m-r-williamson.bsky.social and Theresa Jones), but it’s less clear what’s going on in white matter.
While a lot of responses were shared between the cortical stroke and white matter stroke astrocytes, there were also some really intriguing differences. Top among those: cortical astrocytes were predicted to increase post-stroke vascular remodeling, while white matter astrocytes were not.
October 10, 2025 at 11:13 PM
While a lot of responses were shared between the cortical stroke and white matter stroke astrocytes, there were also some really intriguing differences. Top among those: cortical astrocytes were predicted to increase post-stroke vascular remodeling, while white matter astrocytes were not.
But we didn’t see a correlation when we compared this module to astrocytes in other conditions, like aging or models of Alzheimer’s or Huntington’s disease. This module seems to be generalizable to reactive astrocytes within brain injury and inflammation, but not to all reactive astrocytes.
October 10, 2025 at 11:13 PM
But we didn’t see a correlation when we compared this module to astrocytes in other conditions, like aging or models of Alzheimer’s or Huntington’s disease. This module seems to be generalizable to reactive astrocytes within brain injury and inflammation, but not to all reactive astrocytes.
The genes in this module – also heavily immune-related – show similar changes in other datasets where astrocytes are responding to injury and/or inflammation: spinal cord injury, cortical stab wound, systemic inflammation, other stroke datasets.
October 10, 2025 at 11:13 PM
The genes in this module – also heavily immune-related – show similar changes in other datasets where astrocytes are responding to injury and/or inflammation: spinal cord injury, cortical stab wound, systemic inflammation, other stroke datasets.
There are a lot of similarities between the two: the most reactive astrocytes in both stroke models are heavily involved in immune responses. Using network analysis, we found a module of genes that particularly relates to the level of reactivity, regardless of stroke model.
October 10, 2025 at 11:13 PM
There are a lot of similarities between the two: the most reactive astrocytes in both stroke models are heavily involved in immune responses. Using network analysis, we found a module of genes that particularly relates to the level of reactivity, regardless of stroke model.
We defined zones of reactive astrocytes in mouse models both a large vessel cortical stroke and white matter stroke, using a lot of phenotypic and morphologic analyses, then used those zones for a transcriptomic analysis.
October 10, 2025 at 11:13 PM
We defined zones of reactive astrocytes in mouse models both a large vessel cortical stroke and white matter stroke, using a lot of phenotypic and morphologic analyses, then used those zones for a transcriptomic analysis.
Astrocytes in the white matter are pretty different from astrocytes in the gray matter. So we also wanted to include that layer of complexity – do white matter and gray matter astrocytes respond differently to stroke?
October 10, 2025 at 11:13 PM
Astrocytes in the white matter are pretty different from astrocytes in the gray matter. So we also wanted to include that layer of complexity – do white matter and gray matter astrocytes respond differently to stroke?
We’re interested in both large-vessel strokes as well as small strokes that happen in the white matter tracts of the brain, which are clinically distinct forms of stroke. Small lacunar infarcts in the white matter are one of the underlying pathologies of vascular dementia.
October 10, 2025 at 11:13 PM
We’re interested in both large-vessel strokes as well as small strokes that happen in the white matter tracts of the brain, which are clinically distinct forms of stroke. Small lacunar infarcts in the white matter are one of the underlying pathologies of vascular dementia.
Long story slightly longer: Astrocytes react strongly to any kind of injury, like stroke. We wanted to understand more about the range of reactions – how are astrocytes right next to the stroke responding, and how much do those responses change as you get further away from the injury?
October 10, 2025 at 11:13 PM
Long story slightly longer: Astrocytes react strongly to any kind of injury, like stroke. We wanted to understand more about the range of reactions – how are astrocytes right next to the stroke responding, and how much do those responses change as you get further away from the injury?

