
• 30-day case-fatality rate (CFR) fell or stayed stable (except MSSA ↑ 5.2%).
• 30-day mortality rate rose for most infections (in line with incidence rises).
• Graph ⬇️ with data up to 2022/23 shows CFRs across the infections - P. aeruginosa & MRSA among highest CFRs (23-26%)

• 30-day case-fatality rate (CFR) fell or stayed stable (except MSSA ↑ 5.2%).
• 30-day mortality rate rose for most infections (in line with incidence rises).
• Graph ⬇️ with data up to 2022/23 shows CFRs across the infections - P. aeruginosa & MRSA among highest CFRs (23-26%)
• Black & Asian groups show the highest age-standardised incidence for most infections (except CDI → highest remained in White group).
• Deprivation: the most deprived areas had 1.5-3.1x higher age-sex standardised incidence vs least deprived.
• Black & Asian groups show the highest age-standardised incidence for most infections (except CDI → highest remained in White group).
• Deprivation: the most deprived areas had 1.5-3.1x higher age-sex standardised incidence vs least deprived.
⚠️ ↑ ~50% since 2020/21 to 33.3 per 100k – the highest since 2011/12. Driven by both hospital- and community-onset cases.
See more on recent CDI rises in this technical report:

⚠️ ↑ ~50% since 2020/21 to 33.3 per 100k – the highest since 2011/12. Driven by both hospital- and community-onset cases.
See more on recent CDI rises in this technical report:
↗️ Year-on-year increases continue following the pandemic dip (similar to E. coli), reaching ↑ 12% (unlike E. coli) pre-pandemic levels at 24.2 per 100k.
Community-onset cases were the main driver.

↗️ Year-on-year increases continue following the pandemic dip (similar to E. coli), reaching ↑ 12% (unlike E. coli) pre-pandemic levels at 24.2 per 100k.
Community-onset cases were the main driver.
⚠️ Sharp ↑ 29.5% to 1.9 per 100k vs 2018/19. Reaching a 12-year high & biggest annual increase since surveillance began. Both hospital- and community-onset driving the rise.

⚠️ Sharp ↑ 29.5% to 1.9 per 100k vs 2018/19. Reaching a 12-year high & biggest annual increase since surveillance began. Both hospital- and community-onset driving the rise.
↔️ Incidence has mostly remained steady → 7.8 per 100k in 2024/25.
🏥 Hospital-onset incidence = 4.8 per 100k bed-days.

↔️ Incidence has mostly remained steady → 7.8 per 100k in 2024/25.
🏥 Hospital-onset incidence = 4.8 per 100k bed-days.
↗️ Last year saw the sharpest increase since surveillance began - ↑ 10.3%.
Incidence rose again this year to 23.6 per 100k (+2.9% vs 2023/24).
Largely driven by community-onset infections. While most age-sex groups saw rise, particularly notable among male 75+ years.
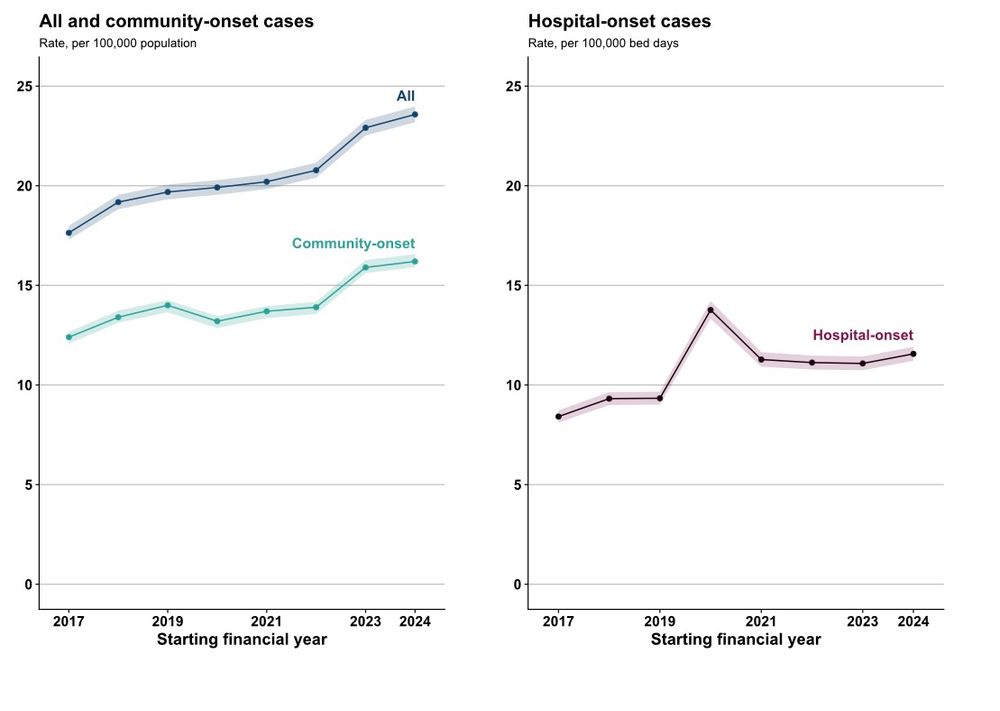
↗️ Last year saw the sharpest increase since surveillance began - ↑ 10.3%.
Incidence rose again this year to 23.6 per 100k (+2.9% vs 2023/24).
Largely driven by community-onset infections. While most age-sex groups saw rise, particularly notable among male 75+ years.
⤴️ In 2024/25, cases rose 17% since 2020/21 → 76.6 per 100k. This rise follows the COVID-19 pandemic dip and is now back to levels similar to those seen in 2018/19.
Most (81%) remain community-onset.

⤴️ In 2024/25, cases rose 17% since 2020/21 → 76.6 per 100k. This rise follows the COVID-19 pandemic dip and is now back to levels similar to those seen in 2018/19.
Most (81%) remain community-onset.
Difficult to say: complex intersection of factors.
People living in more deprived areas and certain ethnic minorities tend to be more affected by:
💔 predisposing comorbidities
💸 poverty
🏫 low educational attainment
⚕️barriers to healthcare
Difficult to say: complex intersection of factors.
People living in more deprived areas and certain ethnic minorities tend to be more affected by:
💔 predisposing comorbidities
💸 poverty
🏫 low educational attainment
⚕️barriers to healthcare

